
- July 4, 2024 | Surprising Vortex Uncovered – Supercomputers Reveal Hidden Secrets of Solar Technology
- July 4, 2024 | A “Word Processor” for Genes – Scientists Unveil Fundamentally New Mechanism for Biological Programming
- July 4, 2024 | The Truth About Fish and Pregnancy: What’s Safe and What’s Not
- July 4, 2024 | Researchers Unveil Natural Solution to Australia’s $280 Million Sheep Problem
- July 4, 2024 | Unusual New Species of Venomous Viper Discovered in China

COVID Gets Airborne – Expert Explains How Viruses Travel Through the Air
By University of California - San Diego January 15, 2022
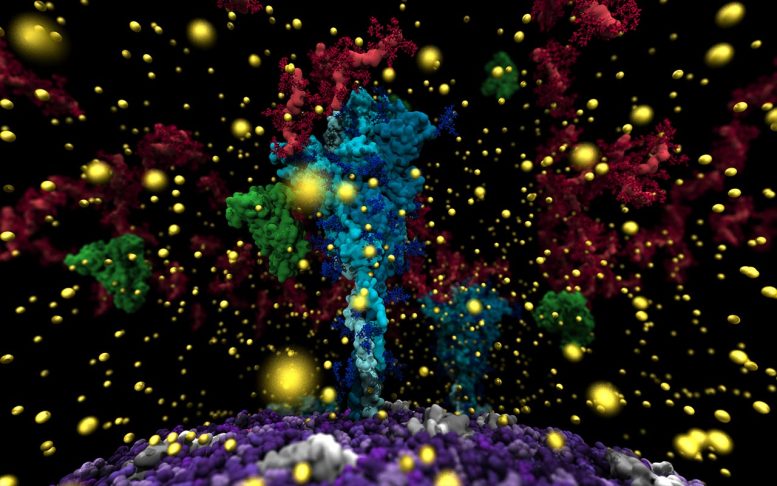
Visualization of the virus’ spike protein (cyan) surrounded by mucus molecules (red) and calcium ions (yellow). The viral membrane is shown in purple. Credit: UC San Diego’s Lorenzo Casalino, the Amaro Lab, and the research team.
UC San Diego develops computer model to aid understanding of how viruses travel through the air.
In May 2021, the Centers for Disease Control officially recognized that SARS-CoV-2 —the virus that causes COVID-19 —is airborne, meaning it is highly transmissible through the air .
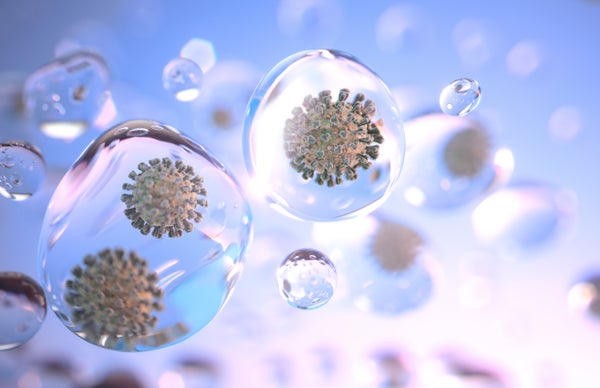
Now University of California San Diego Professor and Endowed Chair of Chemistry and Biochemistry Rommie Amaro, along with partners across the U.S. and around the world, has modeled the delta virus inside an aerosol for the first time.
This work was a finalist for the Gordon Bell Prize, given by the Association for Computing Machinery each year to recognize outstanding achievement in high-performance computing. Amaro led the team that won the prize last year for its work on modeling an all-atom SARS-CoV-2 virus and the virus’s spike protein to understand how it behaves and gains access to human cells .
“It’s wonderful to be a finalist for the Gordon Bell Prize a second year in a row,” stated Amaro. “But more than that, we’re really excited about the potential this work has to deepen our understanding of how viruses are transmitted through aerosols. The impacts could change the way we view airborne diseases.”
Aerosols are tiny. A human hair is approximately 100 microns in diameter. Droplets—think of the spray that comes out of your mouth and nose when you sneeze—are larger than 100 microns and fall to the ground in seconds. In contrast, aerosols—produced simply by breathing and speaking-are everything smaller than 100 microns and can float in the air for hours and travel long distances.
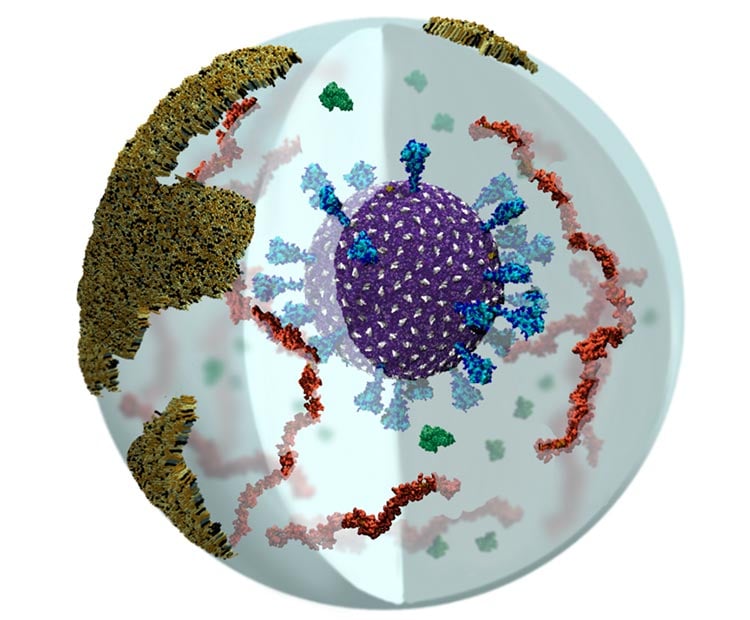
Visualization of delta SARS-CoV-2 in a respiratory aerosol, where the virus is depicted in purple with the studded spike proteins in cyan. Mucins are red, albumin proteins green, and the deep lung fluid lipids in ochre. Credit: UC San Diego’s Abigail Dommer, the Amaro Lab, and the research team.
Kim Prather, Distinguished Chair in atmospheric chemistry and director of the Center for Aerosol Impacts on Chemistry of the Environment (CAICE), has studied sea spray and ocean aerosols extensively. She contacted Amaro several years ago noting that these aerosols had much more than seawater in them.
“The common thinking used to be that ocean aerosols only contained salt water,” Prather stated. “But we discovered there was a ton of ocean-biology inside—living organisms including proteins and viruses. I not only thought Rommie would be interested in studying this, but also thought her work could be really beneficial in helping us gain a better understanding of aerosol composition and movement and airborne survival.”
Amaro’s lab began to develop computer models of what aerosols looked like using Prather’s work in sea spray. These simulations paved the way for Amaro and her group to understand the experimental methods and tools used to study aerosols, generally, as well as develop a useful framework to build, simulate and analyze complex aerosol models.
When SARS-CoV-2 came on the scene in early 2020, she began modeling the virus and was able to show how it infects host cells through a sugary coating called a glycan that covers the spike proteins .
Aerosol scientists always suspected SARS-CoV-2 was airborne, so studying the virus inside an aerosol provided an opportunity to back those suspicions with evidence. Taking the work her lab was already doing with aerosols and the work her lab was also doing with the virus, Amaro put two and two together.
“It’s these fine aerosols that can travel the farthest and move into the deep lung, which can be devasting,” Amaro stated. “There is no experimental tool, no microscope that allows people to see the particles in this much detail, but this new computational microscope allows us to see what happens to the virus—how it moves, how it stays infectious during flight. There is something very powerful about being able to see what something looks like, seeing how components come together—it fundamentally changes the kinds of questions people even think to ask.”
To better understand how the virus moves and lives inside aerosols, Amaro worked with a team of 52 from around the globe, including Oak Ridge National Laboratory, using their Summit supercomputer to simulate the models. Summit is one of the few supercomputers in the world capable of performing these large-scale simulations, which allowed researchers to see aerosols at an unprecedented one billion atoms.
These simulations included more intricate details of the virus’s membranes, as well as visualizations of aerosols. In addition to the SARS-CoV-2 virus, these sub-micron respiratory aerosols also contained mucins, lung surfactant, water, and ions.
Mucins are polymers that line most of the surfaces of the body that are wet, including the respiratory tract and they may work to protect the virus from harsh external elements like sunlight. One of the hypotheses that Amaro’s team is exploring is whether the delta variant of SARS-CoV-2 is more transmissible in part because it seems to interact so well with mucins.
Now that the models have been built, Amaro hopes to formally create an experiment that will test the predictions of aerosolized virus movements. She is also developing tools that will investigate how humidity, wind, and other external conditions affect the transmission and life of the virus in aerosols.
Beyond the immediate needs of learning as much as possible about how SARS-CoV-2 operates, computer models of aerosols can have wide-ranging impacts, including climate science and human health.
“What we learned during the pandemic is that aerosols were one of the main drivers in spreading the virus and that their importance in the transmission of many other respiratory pathogens has been systematically underappreciated,” said Dr. Robert “Chip” Schooley, a professor in the Department of Medicine at UC San Diego School of Medicine. “The more we learn about aerosols and how they host viruses and pollutants, such as soot, that have adverse health impacts, the better positioned we are to create effective treatment and mitigation measures. This benefits the public health and wellbeing of people around the world.”
This work was supported by the NSF Center for Aerosol Impacts on Chemistry of the Environment (CAICE), National Science Foundation Center for Chemical Innovation (NSF CHE-1801971), NIH GM132826, NSF RAPID MCB-2032054, Oak Ridge Computing Facility at Oak Ridge National Laboratory (DOE DE-AC05-00OR22725), Texas Advanced Computing Center Frontera (NSF OAC-1818253), Argonne Computing Facility (DOE DE-AC02-06CH11357), and Pittsburgh Supercomputer Center ( NSF TG-CHE060063). Additional funding provided by RCSA Research Corp. and a UC San Diego Moore’s Cancer Center 2020 SARS-CoV-2 seed grant. This work appears in The Proceedings of SC21, Virtual Event, November 14-19, 2021.
More on SciTechDaily

It’s Not Just COVID-19: Most Respiratory Viruses Actually Spread by Aerosols
First Complete COVID-19 Coronavirus Model Shows Cooperation – “They Work Together”

Caltech’s Nanoparticle Vaccine Protects Against a Wide Range of COVID-19-Causing Variants and Related Viruses

Supercomputer Completes Massive Coronavirus Simulations to Help Design New Drugs and Vaccines
Beyond omicron: scientists set sights on long game of covid evolution, hidden sars-cov-2 “gate” discovered – opens to allow covid infection.
Immediate Detection of Airborne Viruses – Such As COVID-19 – With a Disposable Pathogen Monitoring Kit
COVID Omicron Variant: How Did It Emerge and Is It More Contagious Than Delta? A Virus Evolution Expert Explains
3 comments on "covid gets airborne – expert explains how viruses travel through the air".
I worked in a hospital. No mask if patient didn’t have cough. I tested positive for COVID and intubated on April 7, 2020. I would spend next 98 days in hospital or rehab AND Intubated again. I would have a radial artery repair. I have Long COVID. I have Neuro issues like brain fog (wrong words, wrong order, stopping in middle of sentence,forgetting names of family, friends). I have balance issues, left sided weakness, and nausea episodes every day. I have no memory of most of my journey. I went to my 1st Dr appointment to follow up. I was using a walker. He told me they didn’t expect me to make it. I am alive.
Amazing technology and presentation. I’m left with continued doubts I have about masking. I don’t see how a cloth mask can possibly prevent this type of transmission. Do you have a view on masking whether it be cloth, N95, K95, etc.? I’ve made up my own mind that cloth masks are useless but what does the science reveal? Thanks and really appreciate this information.
Any thing that reduces the number or size of (harmful) particulates that enter the respiratory systems is beneficial. This is not the same as saying it is a flawless filter.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
May 12, 2020
How Coronavirus Spreads through the Air: What We Know So Far
The virus that causes COVID-19 can persist in aerosol form, some studies suggest. But the potential for transmission depends on many factors, including infectiousness, dose and ventilation
By Tanya Lewis
New coronavirus is known to be spread via large droplets that fall to the ground. But whether it can be spread by smaller airborne particles remains unclear.
Getty Images
Several months into a pandemic that has claimed hundreds of thousands of lives and decimated economies around the world, scientists still lack a complete understanding of how the virus that caused it is transmitted. Lockdowns are already easing in some places, and people are preparing to return to a version of work and social life. But a crucial question stubbornly remains: Can the pathogen behind COVID-19 be “airborne”?
For months, the U.S. Centers for Disease Control and Prevention and the World Health Organization have maintained that the novel coronavirus is primarily spread by droplets from someone who is coughing, sneezing or even talking within a few feet away. But anecdotal reports hint that it could be transmissible through particles suspended in the air (so-called "aerosol transmission"). And the WHO recently reversed its guidance to say that such transmission, particularly in “indoor locations where there are crowded and inadequately ventilated spaces where infected persons spend long periods of time with others, cannot be ruled out.” After attending a choir practice in Washington State in early March, dozens of people were diagnosed with or developed symptoms of COVID-19 even though they had not shaken hands or stood close to one another. At least two died. After dining at an air-conditioned restaurant in China in late January, three families at neighboring tables became sickened with the virus—possibly through droplets blown through the air.
To address the prospect of airborne spread of the novel coronavirus, it is first necessary to understand what scientists mean by “airborne.” The term refers to transmission of a pathogen via aerosols—tiny respiratory droplets that can remain suspended in the air (known as droplet nuclei)—as opposed to larger droplets that fall to the ground within a few feet. In reality, though, the distinction between droplets and aerosols is not a clear one. “The separation between what is referred to as ‘airborne spread’ and ‘droplet spread’ is really a spectrum,” especially when talking about relatively small distances, says Joshua Santarpia, an associate professor of pathology and microbiology at the University of Nebraska Medical Center.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Airborne spread has been hypothesized for other deadly coronaviruses, including the ones that cause severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). A handful of studies suggest the new coronavirus, SARS-CoV-2, can exist as an aerosol in health care settings. But much remains unknown about whether the aerosolized virus is infectious and what amount of virus one needs to be exposed to in order to become sick, known as the minimal infectious dose. Even if aerosol transmission does occur, it is not clear how common it is, compared with other transmission routes, such as droplets or surfaces. Uncovering this information is vital, especially given the fact that people can spread SARS-CoV-2 when they have no symptoms.
Perhaps “Is the coronavirus airborne?” is the wrong question. COVID-19 may have the potential for airborne spread, says Stanley Perlman, a professor of microbiology at the University of Iowa. “But whether [this route is] important clinically is really the question one wants to know about,” he says.
Evidence for Aerosol Transmission
Some of the strongest evidence that airborne transmission of the new coronavirus may be possible comes from a study published late last month in Nature . In it, researchers measured the virus's genetic material, or RNA, in aerosols sampled in February and March at two hospitals in Wuhan, China—the city where the outbreak is widely believed to have begun. The researchers found very low levels of airborne viral RNA in the hospitals’ isolation wards and in ventilated patient rooms. But there were measurably higher levels in some of the patients’ toilet areas. They also found high levels of viral RNA in places where medical workers remove protective gear, as well as in two crowding-prone locations near the hospitals. “Our study and several other studies proved the existence of SARS-CoV-2 aerosols and implied that SARS-CoV-2 aerosol transmission might be a nonnegligible route from infected carriers to someone nearby,” says study co-author Ke Lan, a professor and director of the State Key Laboratory of Virology at Wuhan University.
A preprint (not yet published) study led by Santarpia and his colleagues similarly found evidence of viral contamination in air samples and surfaces from rooms where COVID-19 patients were being kept in isolation. “I think there are a lot of us—myself included—who feel very strongly that the airborne route of transmission is very possible,” he says. “I would hesitate to call it proven by any means. But I think there’s mounting evidence to support it.”
Both the Nature study and Santarpia’s paper measured viral RNA, not actual virus, so it is not clear that the material found in aerosols was functionally infectious. “Finding RNA doesn’t tell you [that] you have aerosol spread,” says Perlman, who was not involved in either study.
Another paper, recently published in the New England Journal of Medicine , showed that infectious SARS-CoV-2 virus can remain in aerosols for at least three hours—and for several days on various surfaces—in a laboratory setting. But the amount of viable virus diminished significantly during that time. Scientists do not know the infectious dose of SARS-CoV-2. (For influenza, studies have shown that just three virus particles are enough to make someone sick.)
Overall, most of the evidence that SARS-CoV-2 can become airborne comes from clinical settings—which tend to have a lot of sick people and may host invasive procedures, such as intubations, that can cause patients to cough, generating aerosols. It is not clear how representative of everyday environments these areas are. “There is not much convincing evidence that aerosol spread is a major part of transmission” of COVID-19, Perlman says.
That assessment does not mean it is not occurring, however. Benjamin Cowling, head of the division of epidemiology and biostatistics at the University of Hong Kong’s School of Public Health, says there is a popular misconception that if a virus can spread through the air at all, it must be able to spread over a long range. He gives the analogy of being in a restaurant where someone is smoking: “If the person on the other side of restaurant is smoking, you probably wouldn’t smell it, and you’d never even notice. That’s because the smoke would never reach you,” he says. “It doesn’t mean there’s not smoke produced.” In other words, just because SARS-CoV-2 may not be transmitted over a long range, that does not mean it is not airborne. Like cigarette smoke, aerosol particles spread around a person in a cloud, with the concentration being highest near the smoker and lower as one gets farther away.
Even if aerosols do not travel farther than most droplets, the oft-touted “ six-foot rule ” for social distancing may depend on the circumstances, Cowling says. If there is a fan or air conditioner, infectious aerosols (or even droplets, as was suspected in the case of that restaurant in China) could potentially sicken someone farther away who is downwind.
Some evidence suggests that talking could be a significant mode of viral transmission. A study published on May 13 in Proceedings of the National Academy of Sciences USA used laser light scattering to visualize tiny saliva droplets expelled during speech. The research did not measure droplets with viable SARS-CoV-2 virus. But if one assumes the droplets contain seven million virus particles per milliliter, a minute of loud speech could generate more than 1,000 virus-containing droplets that could hang in the air for eight minutes or more, the researchers write in the study. “There is a substantial probability that normal speaking causes airborne virus transmission in confined environments,” they conclude.
Factors That Affect the Risk of Airborne Spread
Cowling hypothesizes that many respiratory viruses can be spread through the airborne route—but that the degree of contagiousness is low. For seasonal flu, the basic reproduction number, or R 0 —a technical designation for the average number of a people a sick person infects—is about 1.3 . For COVID-19, it is estimated to be somewhere between two and three (though possibly as high as 5.7 ). Compared with measles, which has an R 0 in the range of 12 to 18 , these values suggest most people with the disease caused by SARS-CoV-2 are not extremely contagious.
But there are seeming exceptions, such as the choir practice in Washington State, Cowling says. A CDC report about the event released on May 12 found that of the 61 people who attended the 2.5-hour practice (one of whom had coronavirus symptoms), 32 developed confirmed COVID-19 infections and 20 developed probable ones. The report concluded that “transmission was likely facilitated by close proximity (within 6 feet) during practice and augmented by the act of singing” and that singing “might have contributed to transmission through emission of aerosols, which is affected by loudness of vocalization.” For unknown reasons, some individuals seem to infect many more people than others do. These so-called superspreaders were documented in the SARS outbreak of 2003, too. In what has become known as the 20/80 rule , about 80 percent of infectious-disease-transmission events may be associated with just 20 percent of cases, Cowling notes. “We don’t know how to identify those 20 percent,” he says. “But if we were able to, in some way, then that would be a major advance.”
Ventilation likely also plays an important role in how easily the virus can be transmitted through the air. Indoor spaces probably pose a higher risk than outdoor ones, especially if they are poorly ventilated, Cowling and others say. Crowded areas such as bars, restaurants and subway trains could all be risky—especially if people are asymptomatic and spend long periods of time in such areas. Precautions could include better ventilation, regular cleaning and mask wearing.
Cowling co-authored a study, published in early April in Nature Medicine , of patients with respiratory infections at an outpatient clinic in Hong Kong between 2013 and 2016. This research detected RNA from seasonal coronaviruses—the kind that cause colds, not COVID-19—as well as seasonal influenza viruses and rhinoviruses, in both droplets and aerosols in the patients’ exhaled breath. The paper, led by Nancy Leung, an assistant professor at the University of Hong Kong’s school of public health, found that wearing surgical masks reduced the amounts of influenza RNA in droplets and of seasonal coronavirus RNA in aerosols.
Although the study did not look at COVID-19 specifically, the findings support mask wearing as an effective way to limit transmission of the virus from an infected person—known in medical parlance as source control. There is not much evidence that masks convey protection to healthy people, although it is possible (and may depend on the type of mask). Given the prevalence of asymptomatic infection with COVID-19, however, there is some justification for universal mask wearing to prevent those who do not know they are sick from infecting others. In Hong Kong, which has kept its outbreak relatively under control, masks are worn by the vast majority of the population, Cowling says.
The likelihood of airborne transmission—especially compared with other routes, such as droplets or surfaces—remains unclear. Most researchers still think the new coronavirus is primarily spread via droplets and touching infected people or surfaces. So diligent hand washing and social distancing are still the most important measures people can take to avoid infection.
Leung puts the risks in perspective. Most of what people know about aerosol transmission is from tuberculosis, measles and chickenpox, she says—and these pathogens usually have high transmissibility, with the potential for long-range spread. “The conventional thinking is, therefore, once you mention there’s aerosol transmission, everyone is so worried because [they assume that the virus has] higher transmissibility and that it’s more difficult to control,” she explains. But even if there is airborne transmission, it may only happen at short range—within which other infection routes may be just as likely—or more so. Thus, Leung adds, “having a higher risk of aerosol transmission itself doesn’t necessarily translate to more transmissibility.”
Read more about the coronavirus outbreak from Scientific American here , and read coverage from our international network of magazines here .
Editor's Note (7/9/20): This article was updated in light of the World Health Organization's acknowledgment of potential aerosol transmission of the new coronavirus. The reversal came after more than 200 scientists contributed to an open letter pointing to the cumulative evidence for this type of transmission. The text had previously been amended on May 15 to include new information about droplets spread by talking and about a choir practice in Washington State that sickened many people.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 02 April 2020
Is the coronavirus airborne? Experts can’t agree
- Dyani Lewis
You can also search for this author in PubMed Google Scholar
Since early reports revealed that a new coronavirus was spreading rapidly between people, researchers have been trying to pin down whether it can travel through the air. Health officials say the virus is transported only through droplets that are coughed or sneezed out — either directly, or on objects. But some scientists say there is preliminary evidence that airborne transmission — in which the disease spreads in the much smaller particles from exhaled air, known as aerosols — is occurring, and that precautions, such as increasing ventilation indoors, should be recommended to reduce the risk of infection.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 580 , 175 (2020)
doi: https://doi.org/10.1038/d41586-020-00974-w
Liu, Y. et al. Preprint at bioRxiv http://doi.org/dqts (2020).
Ong, S. W. X. et al. J. Am. Med. Assoc . http://doi.org/ggngth (2020).
Article Google Scholar
Santarpia, J. L. et al. Preprint at medRxiv http://doi.org/dqtw (2020).
van Doremalen, N. et al. N. Engl. J. Med . http://doi.org/ggn88w (2020).
Yan, J. et al. Proc. Natl Acad. Sci. USA 115 , 1081–1086 (2018).
Article PubMed Google Scholar
Cheng, V. C. C. et al. Infect. Control Hosp. Epidemiol . https://doi.org/10.1017/ice.2020.58 (2020).
Download references
Reprints and permissions
Related Articles
- Public health
- Health care
‘Epigenome editor’ silences gene that causes deadly brain disorders
News 27 JUN 24

How blockbuster obesity drugs create a full feeling — even before one bite of food

Ketamine for depression: slow-release pills could make treatment more accessible
Streamlined collaboration can boost CRISPR gene therapies for rare diseases
Correspondence 02 JUL 24

Combined COVID-flu vaccines are coming: Moderna jab clears major test
News 28 JUN 24

‘Vindicated’: Embattled misinformation researchers celebrate key US Supreme Court decision
News 26 JUN 24

Faecal transplants can treat some cancers — but probably won’t ever be widely used
Outlook 04 JUL 24

How Rwandan paediatrician Agnes Binagwaho fights racial stereotypes in global health
Career Q&A 02 JUL 24
Postdoctoral Research Scientist: DNA Replication and Repair in Haematopoietic Stem Cells
An exciting opportunity has arisen for a highly motivated Postdoctoral Research Scientist to join Professor Chapman’s Group, to investigate how DNA...
Oxford, Oxfordshire
University of Oxford, Radcliffe Department of Medicine
Tenure-Track Assistant Professor to the rank of Associate Professor in computational biology
UNIL is a leading international teaching and research institution, with over 5,000 employees and 15,500 students split between its Dorigny campus, ...
Lausanne, Canton of Vaud (CH)
University of Lausanne (UNIL)
Post-doctoral researcher (m/f/d) in Marine Microbial Natural Product Chemistry
GEOMAR Helmholtz Centre for Ocean Research Kiel, Wischhofstraße 1-3, 24148 Kiel, Germany
Helmholtz Centre for Ocean Research Kiel (GEOMAR)
Global Faculty Recruitment of School of Life Sciences, Tsinghua University
The School of Life Sciences at Tsinghua University invites applications for tenure-track or tenured faculty positions at all ranks (Assistant/Ass...
Beijing, China
Tsinghua University (The School of Life Sciences)
Sales Executive, Nature Careers
If you're customer-focused, thrive in sales, and want to impact Europe's job market, join our Nature Careers team !
London - hybrid working model
Springer Nature Ltd
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
CDC confirms COVID-19 virus can spread through airborne transmission indoors
Airborne transmission brings more concerns about gathering indoors, experts say.
After some back-and-forth, the Centers for Disease Control and Prevention again confirmed the virus that causes COVID-19 can be spread through airborne transmission even when people are more than 6 feet away from an infected person, increasing the importance of wearing masks and proper ventilation when gathering indoors.
Airborne transmission is not the primary way the virus spreads, but the CDC today acknowledge it is possible -- particularly in poorly ventilated, indoor spaces.
The update to the CDC's website Monday followed criticism last month after the agency posted information on airborne transmission and then abruptly removed it.
Public health experts had initially expressed relief the agency was posting information that matched the latest science amid reports of political interference in the COVID-19 response. CDC Director Robert Redfield and other CDC officials have said the language was posted accidentally before it finished the agency's scientific review process and that it was an internal error, not a result of outside pressure.
MORE: CDC abruptly removes new guidance on coronavirus airborne transmission
The CDC now says the virus can spread in small droplets or particles that linger in the air, potentially for hours after an infected person has left the space.
The guidance still emphasizes that the primary risk of infection is from coming in close contact with an infected person who could cough or sneeze larger droplets carrying the virus, or from exposure to the virus on surfaces.
The CDC emphasized "limited, uncommon circumstances" when the virus can spread among people more than 6 feet away or after an infected person left the room.

"Today's update acknowledges the existence of some published reports showing limited, uncommon circumstances where people with COVID-19 infected others who were more than 6 feet away or shortly after the COVID-19-positive person left an area. In these instances, transmission occurred in poorly ventilated and enclosed spaces that often involved activities that caused heavier breathing, like singing or exercise," the CDC said in a statement .
But experts in how viruses can travel through the air say the CDC guidance doesn't emphasize enough that transmission at close range can also be through airborne particles, especially since asymptomatic individuals could be spreading the virus only through speech and not the coughing or sneezing that would create larger particles.
MORE: After CDC whiplash, here's what science says about airborne transmission of the coronavirus
Robert Schooley, an infectious disease specialist at the University of California, San Diego, said this makes it even more important for people to wear masks when indoors with people outside your household.
"We've spent a lot of time talking about social distancing as if '6 feet' is a magic number, and the advice people should wear masks only if they can't socially distance is really very poorly thought out advice in the context of aerosol spread," he told reporters on Monday.

"The advice we should be giving people is to wear a mask whenever you're indoors with someone other than your family and move beyond this concept of a magic 6-foot dichotomy of the spread of this virus and the spread of other viruses spread by airborne transmission. As we've seen this week at the White House wearing masks is critical," he said.
A group of experts in aerosolized particles and infectious diseases urged officials to incorporate more of the science on aerosolization into the public health response in a letter published Monday, saying that if symptomatic people are staying home, there should be more emphasis on protecting people from asymptomatic spread through indoor air with proper ventilation and moving events and gatherings outside whenever possible.
"There is overwhelming evidence that inhalation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) represents a major transmission route for coronavirus disease 2019 (COVID-19)," six experts from universities around the country wrote in a letter published in the journal Science on Monday.
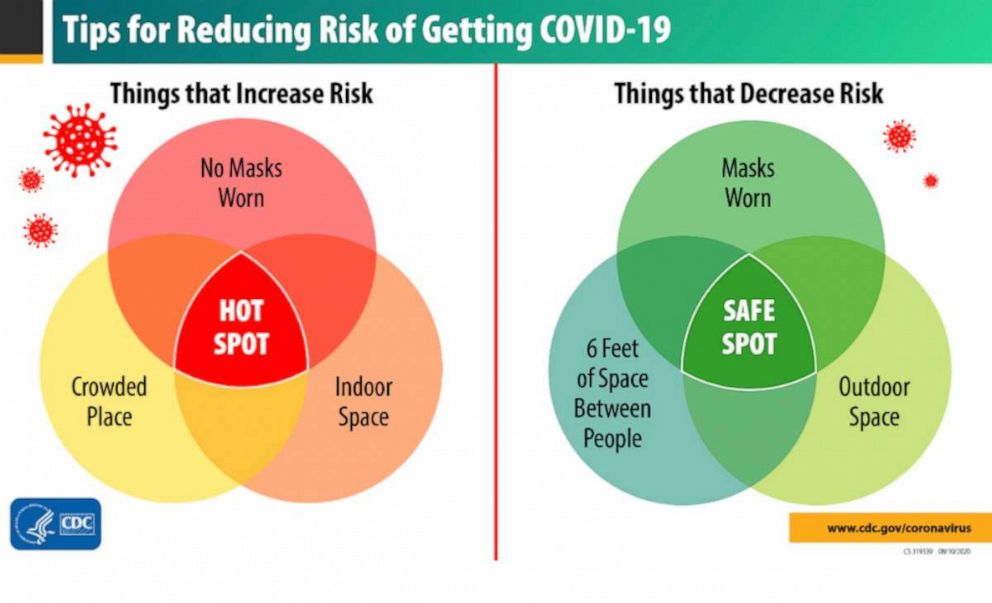
They say that because the most important ways to prevent airborne transmission are by telling people to prioritize outdoor gatherings or improve ventilation indoors with steps like opening windows.
"Knowing it's in the air, acknowledging it's in the air, you can actually fix this problem. It's a very fixable problem," Kimberly Prather, Distinguished Professor of Atmospheric Chemistry at UC San Diego, told reporters on Monday.
The CDC recommends maintaining a distance of at least 6 feet from others, wearing a face mask, avoiding large gatherings and conducting any event or gathering outside as much as possible.
Related Topics
- Coronavirus
Trending Reader Picks

12-year-old attacked and taken by crocodile
- Jul 3, 2:42 AM

Hurricane Beryl: Storm slamming Jamaica
- Jul 3, 9:00 PM

Flight diverts after travelers served spoiled food
- Jul 3, 7:52 AM

Biden said to signal 'open mind' on path forward
- Jul 3, 2:04 PM

Parents at beach with kids die in rip current
- Jun 21, 8:38 AM
ABC News Live
24/7 coverage of breaking news and live events
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
The Coronavirus Crisis
Scientists probe how coronavirus might travel through the air.

Nell Greenfieldboyce

When researcher Josh Santarpia stands at the foot of a bed, taking measurements with a device that can detect tiny, invisible particles of mucus or saliva that come out of someone's mouth and move through the air, he can tell whether the bedridden person is speaking or not just by looking at the read-out on his instrument.
"So clearly the particles that that person is putting out are being breathed in by someone that is five feet away from them, at the foot of their bed," says Santarpia, who studies biological aerosols at the University of Nebraska Medical Center. "Do they contain virus? I don't know for sure."
He and his colleagues are doing their best to find out. Already, using another contraption that looks like a fancy dustbuster, they've sucked up air samples from 11 isolation rooms that housed 13 people who tested positive for COVID-19 infection, all of whom had a variety of mild symptoms.
In those air samples, researchers found the genetic fingerprint of the virus. "It was more than half of the samples that we took. It was fairly ubiquitous," says Santarpia, "but the concentrations were really pretty low."
Finding the genetic material doesn't necessarily mean that there's viable virus that could potentially make someone sick, he cautions. Some preliminary evidence indicates that this might be the case, but the team wants to do more work "and try and be as certain as we possibly can whether or not certain samples had infectious virus in them or not."
They want to know that with a high degree of confidence because the question of whether or not the coronavirus can be "airborne" is extremely contentious right now — and it's a question that has real implications for what people should do to avoid getting infected.
Investigating 'Bioaerosols'
Now, citing Santarpia's results along with other studies, a committee of independent experts convened by the National Academies of Sciences, Engineering, and Medicine has weighed in, in response to a question from the White House Office of Science and Technology Policy about whether the virus "could be spread by conversation in addition to sneeze/cough-induced droplets."
"Currently available research supports the possibility that SARS-CoV-2 could be spread via bioaerosols generated directly by patients' exhalation," says a letter from the committee chair. By bioaerosols, they are referring to fine particles emitted when someone breathes that can be suspended in the air rather than larger droplets produced through coughs and sneezes.
Even if additional research shows that any virus in such tiny particles is viable, researchers still won't how much of it would need to be inhaled to make someone sick. But the committee experts also caution that uncertainty about all this is almost a given—because there's currently no respiratory virus for which we know the exact proportion of infections that come from breathing the virus in versus coming into contact with droplets in the air or on surfaces.
"I personally think that transmission by inhalation of virus in the air is happening," says Linsey Marr , an aerosol scientist at Virginia Tech. But she says so far, health experts have largely discounted the possibility of transmitting this coronavirus in this way.
"I think the public is concerned about this, but the World Health Organization says 'no, the disease is not airborne,'" says Marr.
"From an infection prevention perspective, these things are not 100% black and white. The reason why we say 'droplet' versus 'airborne' versus 'contact' is to give overall guidance on how to manage patients who are expected to be infectious with a specific pathogen," said Dr. Hanan Balkhy , assistant director-general for antimicrobial resistance at WHO, in an interview with NPR earlier this week.
As an expert who worked to contain an outbreak of the deadly MERS coronavirus in Saudi Arabia, she believes that this new virus should behave similarly to other severe coronaviruses — and that means, unless health-care workers are doing invasive procedures like putting in breathing tubes, the virus is expected to primarily spread through droplets.
Droplets are larger respiratory particles that are 5 to 10 micrometers in size. Those are considered "big," even though a 5 micrometer particle would still be invisible to the naked eye. Traditionally, those droplets are thought to not travel more than about three feet or so after exhalation. That would mean the virus can only spread to people who get close to an infected person or who touch surfaces or objects that might have become contaminated by these droplets. This is why public health messages urge people to wash their hands and stand at least 6 feet away from other people.
An "airborne" virus, in contrast, has long been considered to be a virus that spreads in exhaled particles that are tiny enough to linger in the air and move with air currents, letting them be breathed in by passersby who then get sick. Measles is a good example of this kind of virus — an exhaled measles pathogen can hang suspended in a room for a couple hours after an infected person leaves.
The reality of aerosol generation, however, is far more complex than this "droplet" versus "airborne" dichotomy would suggest, says Marr. People produce a wide range of different-sized particles of mucus or saliva. These particles get smaller as they evaporate in the air and can travel different distances depending on the surrounding air conditions.
"The way the definitions have been set up, this "droplet" vs "airborne" distinction, was first established in the 1950s or even earlier," says Marr. "There was a more limited understanding of aerosol science then."
Even a 5 micrometer droplet can linger in the air. "If the air were perfectly still, it would take a half hour to fall from a height of 6 feet down to the ground. And, of course, the air isn't perfectly still," says Marr. "So it can easily be blown around during that time and stay in the air for longer or shorter."
What's more, coughs and sneezes create turbulent clouds of gas that can propel respiratory particles forward.
"For symptomatic, violent exhalations including sneezes and coughs, then the droplets can definitely reach much further than the 1 to 2 meter [3 to 6 feet] cutoff," says Lydia Bourouiba , an infectious disease transmission researcher at MIT, referring to the distance typically cited as safe for avoiding droplet-carried diseases.
How Far Can Droplets Travel?
In fact, studies show that "given various combinations of an individual patient's physiology and environmental conditions, such as humidity and temperature, the gas cloud and its payload of pathogen-bearing droplets of all sizes can travel 23 to 27 feet," she wrote in a recent article published online by the Journal of the American Medical Association.
At a briefing by the White House's coronavirus task force on Tuesday, a reporter asked Dr. Anthony Fauci , head of the National Institute of Allergy and Infectious Diseases, about the potential for the coronavirus to travel 27 feet.
"This can really be terribly misleading," said Fauci, who then reared his head back and mimicked making an enormous sneeze. "If you go way back and go, 'Achoo!' And go like that, you might get 27 feet. So when you see somebody do that, get out of the way."
Fauci went on to say he was "disturbed" by headlines about the virus traveling such distances "because that's misleading. That means that, all of a sudden, the 6-foot thing doesn't work."
The virus traveling distances that might be achieved after a vigorous sneeze is "not what we're talking about" when it comes to social distancing, Fauci said, defending the 6-foot guideline.
WHO, in its general communications with the public on such platforms as Twitter, has stated that the virus "is NOT airborne" and that it is mainly transmitted "through droplets generated when an infectious person coughs, sneezes or speaks."
"Transmission of COVID-19 is through droplets, it is not airborne," said Dr. Maria Van Kerkhove, the WHO's technical lead for COVID-19, at a recent press briefing. "Therefore someone who has these small liquid particles that come out of their mouth; they travel a certain distance and then they fall so that's why we recommend the physical distance, to be separated so that you remove the opportunity for that virus to actually pass from one person to another."
And in its technical guidance on how the virus is transmitted, WHO says that protections against airborne transmission are only needed for health-care workers when they do medical procedures which might be anticipated to produce smaller respiratory droplets that could then be inhaled.
That position has been criticized by some experts on virus transmission, however, who say so little is known about this virus that it is better to be cautious and recommend that health-care workers use N95 masks and other kinds of more protective gear for all patient care whenever possible, especially given the emerging bits of evidence that airborne transmission is a possibility.
But WHO has defended its stance.
"This is not the WHO's opinion on its own. The WHO provides such guidelines through its networks of scientific experts from around the world," Balkhy told NPR.
"It can be inhaled if you are very close to the patient, if you are creating aerosolization," says Balkhy. But she said past clinical experience with other severe coronaviruses, SARS and MERS, supports the idea that these viruses mainly spread via droplet transmission.
In order to conclude otherwise, she said, "we need to have the evidence that it actually is being spread through a specific route that we're not seeing right now."
New Report On Airborne Transmission
Some of the strongest evidence that an airborne route of transmission might be possible for this virus comes from a report published last month by the New England Journal of Medicine that described mechanically generating aerosols carrying the SARS-CoV-2 virus in the laboratory. It found that the virus in these little aerosols remained viable and infectious throughout the duration of the experiment, which lasted 3 hours.
WHO mentioned this study in its recent review of possible modes of transmission and noted that "this is a high-powered machine that does not reflect normal human cough conditions ... this was an experimentally induced aerosol-generating procedure."
It may have been artificial, says Marr, but "the conditions they used in that laboratory study are actually less favorable for survival compared to the real world. So it's more likely that the virus can survive under real world conditions."
Humans definitely produce droplets that can dry down to the sizes that were tested in that study, says Santarpia. "Do ill people with this disease produce respiratory droplets containing the virus which dry down to those sizes? That I don't know," he says. "That's the sort of piece of data that I am trying to get right now."
Another important piece of information for understanding the risk of airborne transmission of this disease would be knowing how much of the virus a person has to inhale in order to actually fall ill.
"We're starting to answer the questions about how stable is this as an aerosol. We're starting to answer the questions about what kind of aerosols are people producing that have infectious virus in them," says Santarpia. "The last piece of that is the infectious dose, or how many virus particles do you have to ingest or inhale to become sick."
He thinks it is possible that some form of airborne spread is playing a role in the transmission of this virus.
"In my opinion, it's probably more than just droplet," says Santarpia, adding that intuitively it does not seem to him "that this is just like large droplets that just sort of have ballistic trajectories and land inside your mouth that are causing disease."
Still, he says, "one of the reasons we are doing the work that we are doing is that this is science and we look for proof."
The 6 Foot Recommendation
Generally speaking, researchers say, the 6-foot distance recommendation seems reasonable.
But if enough people gather in a room that has little or no ventilation, it's possible that even large droplets might accumulate in the air.
"Given what we know so far about this virus, 6 feet is OK if it's not crowded. But if you are in a room or somewhere where there is a person every 6 feet, then you could have enough virus in the air that I would be concerned," says Marr.
Something like that might have happened when a choral group in Washington state got together to sing, and ended up with dozens of cases of COVID-19 despite the fact that members of the group were careful not to touch each other or stand close.
"The simplest explanation is that it was being transmitted through the air," she says, noting that people should ventilate buildings and that concentrations of particles are less likely to build up outdoors.
She personally likes to stay 10 feet away from people, and is thinking of wearing some kind of mask for trips to the grocery store.
But even if scientific studies eventually prove that there's an airborne component to transmission, says Santarpia, that doesn't mean that you run the risk of contracting the disease from great distances, like if some stray, lonely virus particle floated into your path from way down the street.
"I just don't think that's realistic," he says, adding that he's assured his aunt that it's fine for his 95-year-old grandmother to sit outside on the porch to enjoy a sunny day.
- Share full article
Advertisement
Supported by
Airborne Coronavirus: What You Should Do Now
How to protect yourself from a virus that may be floating indoors? Better ventilation, for starters. And keep wearing those masks.

By Apoorva Mandavilli
The coronavirus can stay aloft for hours in tiny droplets in stagnant air , infecting people as they inhale, mounting scientific evidence suggests.
This risk is highest in crowded indoor spaces with poor ventilation, and may help explain super-spreading events reported in meatpacking plants, churches and restaurants.
It’s unclear how often the virus is spread via these tiny droplets, or aerosols , compared with larger droplets that are expelled when a sick person coughs or sneezes, or transmitted through contact with contaminated surfaces , said Linsey Marr, an aerosol expert at Virginia Tech.
Aerosols are released even when a person without symptoms exhales, talks or sings, according to Dr. Marr and more than 200 other experts, who have outlined the evidence in an open letter to the World Health Organization .
What is clear, they said, is that people should consider minimizing time indoors with people outside their families. Schools, nursing homes and businesses should consider adding powerful new air filters and ultraviolet lights that can kill airborne viruses.
Here are answers to a few questions raised by the latest research.
What does it mean for a virus to be airborne?
For a virus to be airborne means that it can be carried through the air in a viable form. For most pathogens, this is a yes-no scenario. H.I.V., too delicate to survive outside the body, is not airborne. Measles is airborne, and dangerously so: It can survive in the air for up to two hours.
For the coronavirus , the definition has been more complicated. Experts agree that the virus does not travel long distances or remain viable outdoors. But evidence suggests it can traverse the length of a room and, in one set of experimental conditions, remain viable for perhaps three hours .
Listen to ‘The Daily’: Four New Insights About the Coronavirus
Hosted by michael barbaro, produced by by alexandra leigh young and austin mitchell, and edited by larissa anderson, a look at what scientists have learned about how the virus takes hold in the body and where the risk of infection is highest..
From The New York Times, I’m Michael Barbaro. This is “The Daily.”
Today: As infection rates break new records across the U.S. this July 4 weekend, four new insights into the virus from my colleague, science reporter Donald G. McNeil Jr. It’s Monday, July 6.
Let me start by, Donald, saying happy 4th of July.
How did you spend it?
Saturday, I played softball in the morning — socially distant softball.
In New York City?
In New York City. Yeah, Riverside Park. And then we went to dinner last night in a friend’s backyard on Long Island, where we all sat as couples together, but six feet apart from each other, and sort of took turns going up to the table to get to the food, and sat, and had a really nice time.
I have to imagine that even a socially distanced meal with you is challenging, in that I think I would feel quite seen and judged, given your role.
I mean, I do tend to say six feet, six feet, six feet, a lot at people.
Because masks give people a false sense of security. I mean, this is a big thing on the softball field, is that people would both put on masks and they’d sit next to each other in the dugout, making up the batting order and stuff like that. And I’d go, no! Air leaks out of the side of your masks. And you’re not always wearing masks. Sometimes you’re wearing it as a sort of a Captain Ahab blue beard under your chin. So it’s better to stay six feet apart. That way if your mask —
Do your remember a couple seconds ago how you asked me why it might be challenging to have a —
— a meal with you?
All right. [LAUGHTER]
All right, touche, touche.
So everything you just described, of course, is occurring in New York, where the infection rate has been generally declining or at least stabilizing. So let’s talk about the state of the pandemic in the rest of the country. I wonder if you can give us a quick status update on this end of July 4 weekend.
OK. I think it’s 39 states now have cases going up. And it’s hitting hardest in the South and in the West. Texas, Florida, Arizona, California, a number of other states. And it’s exactly what was predicted back in May when states were debating opening by Memorial Day. All public health experts said, if you open up when your case counts are rising, they’re going to continue rising and start rising even faster. And now we’re seeing that.
For example, in Houston, doctors who knew the situation in New York are saying that what’s happening there looks like what happened in New York in early April. Finding new beds, finding ventilators, lots of patients who were sick, patients who were on oxygen. Not as many dying yet, but with people on oxygen and on ventilators they may find themselves in the situation where they have to park refrigerated trucks behind hospitals to hold the bodies, as they did in New York.
So Donald, correct me if I’m wrong. I think the U.S. is at about 50,000 infections a day right now. Dr. Anthony Fauci said we could get up to 100,000. And if that’s the case, what do we expect the attendant death count to start to look like in the U.S.? I assume that’s going to catch up with that.
Yeah, it’ll catch up with it. I mean, but there’s no reason to believe that 100,000 is the upper limit. It all depends on how much social distancing we practice. I mean, this is the dance. And do you close bars and restaurants? Do you open or close schools? Do you wear masks? How much attention do people pay to the directions you give them? How much do they practice good social distancing. That very much affects the rate of spread of the virus.
Well, with that in mind, those big questions of kind of how we proceed through the rest of this pandemic, you have been doing a lot of reporting about the latest learnings and insights into the virus that will very much guide how we answer those questions. And we want to talk through those with you. So where do you think we should start?
Some of these insights are really more theories with some evidence to them. And some there’s quite a bit of confidence in. So we probably ought to start with something that there’s a pretty high degree of confidence in among doctors.
And what is that?
When this all started, we thought of it as a lung disease, a respiratory disease, because the first cases we heard about, people got pneumonia. And that of course reminded us that the model for this disease was the 1918 influenza epidemic. But we’re learning that this coronavirus is very different from an influenza virus.
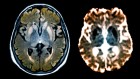
The influenza viruses attach to receptors in the lungs and the airway. This gets into the body through the airway, through the lungs. But it really attaches to the insides of the blood vessels. And so that makes it a vascular disease, a blood vessel disease.
And what are the implications of a virus like this being a vascular disease, a blood vessel disease, and not just a respiratory disease?
It means it affects every organ in the body that has lots of fine blood vessels in it, and not even just organs.
I mean, so it affects the lungs, which are the filter where the air gets into the blood, and you have lots of little fine blood vessels surrounding the little sacs at the ends of your breathing tubes. It attacks the kidneys, because that’s the filter where the urine comes out of the blood. So you have very fine networks of blood vessels there. It attacks the gut, because you have a network of blood vessels in your gut where food gets into your body. It attacks the brain, because you have lots of fine blood vessels in the brain. It doesn’t attack the nerve cells in the brain, which most of the brain is made of. It doesn’t attack the muscle cells in the heart. But it attacks the blood vessels that go through all those other parts.
And so when they do autopsies they find thousands of tiny little blood clots all over the body. We have lots of people who have strokes. And as those blood clots clot up blood vessels to small areas of the brain, you may get dementia or disorientation. And then in kids, when you have ‘Covid toes’ in teenagers and young adults, this is the little capillaries in the hands and feet getting blocked, and getting this inflamed, painful, red or purple toe and finger syndrome. So it’s more complicated to deal with a disease that can travel to any organ in the body.
So how does this new insight about the coronavirus, how does it change the way we are going to approach the pandemic?
Before, the main thing you’re looking for when you’re looking to see if somebody is having a problem is their blood oxygen level. Because you’re assuming that their problem is going to be pneumonia. But if you realize that the problem could be kidney damage, heart damage, you do a whole different battery of blood tests.
So what you’re saying is that doctors who previously were diagnosing Covid-19 through a set of well-established symptoms now need to expand that set of symptoms pretty broadly. Because it turns out this is looking to be vascular, not respiratory.
Yeah, that’s right. It means that virtually anybody who comes into a doctor’s office feeling sick might have the coronavirus. If they come in with symptoms of a stroke, it might be Covid. If they come in with symptoms of a heart attack, it might be Covid. If they come in with what seems like arthritis in their feet, it might be Covid toe.
And because we often don’t have enough tests, or it takes a long time to get test results, the patient’s at a real disadvantage. Because if you don’t know your patient has coronavirus, whatever symptom they’ve got now might become greater, might spread to other organs. So the problem in your toes might literally spread to your kidneys or your brain. And you want to know that that patient has a disease that can spread throughout the body.
In other words, more testing, fast testing becomes more imperative once we have learned that so many symptoms may actually be a sign of Covid-19.
Absolutely.
OK. So what is the next big new insight we have into the coronavirus?
Well, people are always asking, is the virus mutating? Is it becoming different? And the answer is yes. This virus always mutates. It makes one mutation about every two weeks.
The question is are any of those mutations important. And most of them aren’t. Most of them don’t change the function of the virus at all. But there has been one mutation that has become the object of a great deal of interest. We know for sure that there are sort of two general clades of the virus, the Wuhan strain and the other one called the Italian strain or sometimes a European strain. Now, the Wuhan strain is obviously the original one. That’s where the virus started. But it went around Asia. Then it went to Iran. Then it went to Italy. And in Italy sometime in February, presumably, this mutation took place. Now, it has definitely not made the virus more dangerous, more lethal, more likely to kill you. But it appears to have made it more transmissible.
Well, it appears that it transmits between people five to 10 times more easily. Now, this is in dispute. But there’s been work done in cells in the laboratory where they infected them with the two different strains. And the mutation in the Italian strain seems to make the spikes on the outside of the virus — the spikes of the corona — more stable. Better able to infect. And so that they appear to be five to 10 times more capable at infecting cells as the old Wuhan version.
So the strain of this virus that has a better spike — the Italian strain — and is therefore more transmissible, is crowding out the previous strain, because it’s just doing a better, more effective job of infecting people.
Yeah, that’s right. It’s the natural progression for a virus. It’s the way they tend to go.
What do you mean?
Well, viruses, over the course of infecting lots of hosts, tend to become less lethal to those hosts and more transmissible. Like, for example, if I have the virus and it mutates inside me, and it turns into a more deadly strain, I’ve now got two strains. And I pass on that virus to two people, the person who gets the more deadly strain is more likely to go home, go to bed and die. Whereas the person who gets the less lethal, more transmissible strain is going to go out to a disco and infect 40 people.
And if you do that enough times in the course of the virus, the virus always sort of naturally moves in the direction of the more transmissible, less lethal one, because that’s the one that spreads whenever it’s given that kind of fork in the road.
And so this is what happened in 1918. The virus started off extremely deadly. It blew through an enormous chunk of the population, probably 60 to 70 percent of all the people in the world. And then it disappeared for a while. Then it turned up in pigs, and it was a pig virus for a while. And then when enough humans who’d never had the virus were born, it reappeared in people. But it reappeared as the H1N1 seasonal flu, the one that we know about as one of the seasonal flus every year. But that became less lethal and more transmissible. And basically all viruses do that. And we might be beginning to see the very first hints of that happening with this virus.
So if I’m in Texas or Arizona right now and I’m testing positive for Covid-19, it sounds quite likely that I’ve gotten the Italian mutation of this virus, right? And that means I’m quite likely to spread it to somebody else and not have the most horrible symptoms. So does that partly help explain why infection rates are rising so rapidly in the U.S.?
Well, infection rates are rising rapidly in the U.S. more because of human behavior than because of any changes in the virus. I think it’s wishful thinking to think that this virus is not dangerous. It’s really dangerous, and it’s highly transmissible.
But because the Italian version of the virus spreads more effectively, that does suggest that the virus is becoming better at doing the thing it was designed to do, which is to infect lots and lots of people.
Yes. But I mean, the Italian version versus the Wuhan version isn’t the dead end. There are going to be many more mutations. It mutates every two weeks. There may be other mutations turning up in the virus that turn out to be important. And we may call those the Texas strain or the California strain, or whatever.
But we don’t know them yet. There’s a lot of disagreement about this among scientists as to whether or not it really is more transmissible. And there’s zero agreement that it — not even really any thought that it’s less dangerous. That completely remains to be seen.
We’ll be right back.
So Donald, what is the next big new understanding we have into the virus at this point?
Well, there’s more and more confirmation that you are much safer outdoors than you are indoors. There’s a study in China that looked at 318 clusters of transmission. And only one case involved outdoor transmission. And that was between two neighbors who had a long conversation with each other. And there’s recently been another study from Japan that suggests that your chances of getting the virus indoors are 20 times as high as it would be outdoors.
And what are these studies finding about why exactly that is? I think we all have some understanding that when you’re outside the virus is just going to disperse and become more diffuse. Is that as complicated as it is?
Well, there’s always a little bit of wind outside. Humidity also makes droplets fall out of the air. But mostly it’s the wind. And when people talk within a few feet of each other, especially when they talk loud, or when they laugh, or when they sing or shout or do anything like that, you put out this kind of invisible mist of little tiny droplets that spews out of your mouth and sort of hangs around your head. But it also drifts towards the other person. And so you’re sitting inside each other’s droplet cloud. And those little tiny droplets, even if you’re not feeling the other person in effect spitting on your face, that droplet cloud can hold enough virus to transmit the disease from one person to the other.
And indoors when there’s no windows open, it can sort of drift through the room, more or less at head level, and go past one person after another at a cocktail party or inside a bar like that. And each person inhaling a little bit of that droplet cloud, until the disease has spread to 20, 30, 40 people. Whereas outdoors, the breeze just blows that away. So standing six feet away outdoors, even without masks, is considered safe.
This is the idea that the virus becomes aerosolized. And you’re saying that indoors, that poses a very significant danger. Outdoors, because of wind, nowhere near as much.
Yeah, that’s right.
So if being outdoors is less risky, and it’s now been clinically shown, I wonder if that explains something you mentioned the last time that we spoke, which is that you did not have a tremendous amount of fear that these protests that have occurred all over the United States over race and policing, that they would be a major source of infection. And is that because they occurred outdoors? And is it so far the case that they haven’t led to a meaningful spike in infections?
We have not seen any big spike in infections in the cities where most of the protests took place. So it looks like they didn’t lead to a lot of transmission. That doesn’t imply that everything is safe just because it’s outdoors. The important thing is how far apart people are when they’re outdoors. So sitting right next to somebody else in front of a stage at Mount Rushmore, for example, where the chairs are zip tied together, is not safe. Masks or no masks, you still really want to try to keep six feet distance.
Donald, a couple of moments ago you mentioned the danger of being indoors because of this aerosolized virus mist that is not as great a danger outdoors. But I want to linger on this question of the indoors for a moment. Because the more we think about it, that aerosolized mist would seem to make any indoor activity inherently dangerous. I wonder if that’s an accurate assessment?
Yes. I mean, we’ve seen transmission of virus to large numbers of people in funerals, in choir practices, at birthday parties, inside bars, in business meetings. Virtually any kind of indoor environment you can imagine, there have been super spreader events. There may be ways to eventually make indoor spaces safer. There’s going to be no way to make them completely safe.
And all this talk about what’s safe to do indoors brings us to really the most important question, which is the most important indoor space we want to get functioning again, which is schools. Can kids go to school safely? And again, the science isn’t firm yet. But there are more and more hints that it may be safe, or pretty safe, to open the schools in the fall, especially for very young kids.
There’s growing evidence that kids are not big transmitters of the virus to adults. Denmark opened its schools in April. Did not see a big spike up in cases. Finland opened its schools in May. Did not see a big spike up in cases. Even from the beginning in China, the Chinese said, every time they looked at clusters in families, almost never did they see a case where the child, particularly the youngest child, was the one who introduced the virus into the family. Usually it was parent infecting the kids, not the other way around.
We know that kids are big transmitters of flu viruses. And they do it because they cough and sneeze like crazy. But if the biggest symptom that they’re getting is inflammation, rather than coughing and sneezing, — and that’s the case; kids tend to get more sort of cranky, inflammatory, unpleasant manifestations of the disease, rather than something that looks like a cold. Then it would make sense that that might be a reason why they’re not big transmitters.
And what is this new insight about kids being less likely to transmit mean for the teachers who are going to stand or sit in front of them all day? Does it mean that an adult teacher in a school is pretty safe teaching? Or does it not mean that at all?
I don’t think we know the answer to that yet. I mean, schools — you’re bringing together a lot of kids. But schools also bring together a lot of adults. Teachers, staff, parents picking up the kids, things like that. So schools are not going to be completely safe under any circumstances.
But opening schools is so important to society, much more important than opening restaurants, much more important than opening movie theaters. It probably needs to be done really carefully. Not just all back into the classroom, 30 kids to a classroom, at all. But it looks like it could be done. And that’s really important. Because it’s important for the kids, for their development, for their feeding, for their socialization. And it’s also important for the parents. Parents can’t go back to work if they’re stuck at home with their kids. So it’s a crucial part of getting both the economy going and just the health of kids and health of parents.
So of all the insights that you have shared today, this one seems like the silver lining. That reopening schools may be a somewhat safe undertaking.
Yeah. And that would be very good news for us.
Because if I’m being candid, everything else you have said sounds pretty bad, right? I mean, it seems to be vascular, not respiratory. So it’s going to be easy to miss symptoms. It seems it’s becoming more transmissible through mutations. And the indoors presents very significant threats for non-kids because of this aerosolized mist. And once the temperature drops, which it will do in a few months, and tens of millions of us are suddenly stuck indoors, then we’re in for a lot of trouble.
Yeah, and the number of cases per day could rise well over 100,000 if we’re not careful. So yeah, I guess, it’s mostly bad news.
Sorry. I’m hoping that the fact that the virus is becoming more transmissible also means that it will become less lethal, which would be good news. But it hasn’t done that yet. So more transmission of a virus that’s already bad is not a good thing. No question about it.
And all these things that we have just talked about would also seem to reinforce the need, not just for social distancing, but for these government-mandated lockdowns. I mean, specific requirements that say, don’t go to a bar. Don’t go to a restaurant. And those will become even more urgent as the warm weather yields to cold weather.
Yeah. We have to realize we are just in the opening phases of this pandemic. I mean, this is the second inning. And there’s still — there’s more than 120,000 people dead. So we are doing the dance in, dance out of various forms of lockdown. But we need to get to the point where we’re all basically dancing to the same music. Where all governors accept the notion that when they have a problem that’s getting out of control in their state, they react quickly.
And if they do that, they will save lives of their own citizens. And I think we’re beginning to see that.
In places like Texas, places like Arizona, places like Florida the governors have made major about-faces in the last couple of weeks. And they’re getting the science that the thing you do today doesn’t produce good effects until a month from today, because the people who got infected yesterday are the ones who are going to be in your hospital three weeks from now. So they’re beginning to catch on.
But we need to arrive at sort of a common understanding that we don’t all have to move in lockstep as a nation, but at the crucial moments we need to take similar steps to save lives.
Thank you, Donald. We appreciate it.
Thank you. I was glad to be here.
Here’s what else you need to know today.
In our schools, our newsrooms, even our corporate boardrooms, there is a new far-left fascism that demands absolute allegiance.
In a pair of back-to-back speeches over the weekend, President Trump delivered harsh attacks against what he called the radical far-left forces who are protesting police brutality and tearing down monuments to America’s racist past, describing them as a threat to American values and heritage.
If you do not speak its language, perform its rituals, recite its mantras and follow its commandments, then you will be censored, banished, blacklisted, persecuted and punished. It’s not going to happen to us.
The Times reports that the speeches, delivered in front of Mount Rushmore and the White House, signaled that Trump would seek, once again, to exploit racial and cultural divisions in an effort to win re-election.
I am here as your president to proclaim before the country and before the world this monument will never be desecrated. These heroes will never be defaced. Their legacy will never, ever be destroyed. Their achievements will never be forgotten. And Mount Rushmore will stand forever as an eternal tribute to our forefathers and to our freedom.
Neither event enforced social distancing rules. And both were held despite pleas from public health officials that they be canceled to avoid spreading the coronavirus.
That’s it for “The Daily.” I’m Michael Barbaro. See you tomorrow.
How are aerosols different from droplets?
Aerosols are droplets, droplets are aerosols — they do not differ except in size. Scientists sometimes refer to droplets less than five microns in diameter as aerosols. (By comparison, a red blood cell is about five microns in diameter; a human hair is about 50 microns wide.)
From the start of the pandemic, the W.H.O. and other public health organizations have focused on the virus’s ability to spread through large droplets that are expelled when a symptomatic person coughs or sneezes.
These droplets are heavy, relatively speaking, and fall quickly to the floor or onto a surface that others might touch. This is why public health agencies have recommended maintaining a distance of at least six feet from others, and frequent hand washing.
But some experts have said for months that infected people also are releasing aerosols when they cough and sneeze. More important, they expel aerosols even when they breathe, talk or sing, especially with some exertion.
Scientists know now that people can spread the virus even in the absence of symptoms — without coughing or sneezing — and aerosols might explain that phenomenon.
Because aerosols are smaller, they contain much less virus than droplets do. But because they are lighter, they can linger in the air for hours, especially in the absence of fresh air. In a crowded indoor space, a single infected person can release enough aerosolized virus over time to infect many people, perhaps seeding a superspreader event .
For droplets to be responsible for that kind of spread, a single person would have to be within a few feet of all the other people, or to have contaminated an object that everyone else touched. All that seems unlikely to many experts: “I have to do too many mental gymnastics to explain those other routes of transmission compared to aerosol transmission, which is much simpler,” Dr. Marr said.
Can I stop worrying about physical distancing and washing my hands?
Physical distancing is still very important. The closer you are to an infected person, the more aerosols and droplets you may be exposed to. Washing your hands often is still a good idea.
What’s new is that those two things may not be enough. “We should be placing as much emphasis on masks and ventilation as we do with hand washing,” Dr. Marr said. “As far as we can tell, this is equally important, if not more important.”
Should I begin wearing a hospital-grade mask indoors? And how long is too long to stay indoors?
Health care workers may all need to wear N95 masks, which filter out most aerosols. At the moment, they are advised to do so only when engaged in certain medical procedures that are thought to produce aerosols.
For the rest of us, cloth face masks will still greatly reduce risk, as long as most people wear them. At home, when you’re with your own family or with roommates you know to be careful, masks are still not necessary. But it is a good idea to wear them in other indoor spaces, experts said.
As for how long is safe, that is frustratingly tough to answer. A lot depends on whether the room is too crowded to allow for a safe distance from others and whether there is fresh air circulating through the room.
[ Like the Science Times page on Facebook. | Sign up for the Science Times newsletter. ]
What does airborne transmission mean for reopening schools and colleges?
This is a matter of intense debate. Many schools are poorly ventilated and are too poorly funded to invest in new filtration systems. “There is a huge vulnerability to infection transmission via aerosols in schools,” said Don Milton, an aerosol expert at the University of Maryland.
Most children younger than 12 seem to have only mild symptoms, if any, so elementary schools may get by. “So far, we don’t have evidence that elementary schools will be a problem, but the upper grades, I think, would be more likely to be a problem,” Dr. Milton said.
College dorms and classrooms are also cause for concern.
Dr. Milton said the government should think of long-term solutions for these problems. Having public schools closed “clogs up the whole economy, and it’s a major vulnerability,” he said.
“Until we understand how this is part of our national defense, and fund it appropriately, we’re going to remain extremely vulnerable to these kinds of biological threats.”
What are some things I can do to minimize the risks?
Do as much as you can outdoors. Despite the many photos of people at beaches, even a somewhat crowded beach, especially on a breezy day, is likely to be safer than a pub or an indoor restaurant with recycled air.
But even outdoors, wear a mask if you are likely to be close to others for an extended period.
When indoors, one simple thing people can do is to “open their windows and doors whenever possible,” Dr. Marr said. You can also upgrade the filters in your home air-conditioning systems, or adjust the settings to use more outdoor air rather than recirculated air.
Public buildings and businesses may want to invest in air purifiers and ultraviolet lights that can kill the virus. Despite their reputation, elevators may not be a big risk, Dr. Milton said, compared with public bathrooms or offices with stagnant air where you may spend a long time.
If none of those things are possible, try to minimize the time you spend in an indoor space, especially without a mask. The longer you spend inside, the greater the dose of virus you might inhale.
Apoorva Mandavilli is a reporter focusing on science and global health. She is the 2019 winner of the Victor Cohn Prize for Excellence in Medical Science Reporting. More about Apoorva Mandavilli
Is Coronavirus Airborne? What To Know About Whether Or Not COVID-19 Can Stay In The Air
The good news is experts don't think the viral particles can travel very far (whew).

- Recent research suggests that contagious novel coronavirus particles can linger in the air for a few hours.
- Health officials recently said that new coronavirus particles can become airborne from talking or even just exhaling.
- Infectious disease experts still do not think that COVID-19 viral particles spread across far distances.
As social distancing has become the new normal amid the novel coronavirus pandemic , you may have wondered whether it's still a potential risk to share space and cross paths even at a distance. After all, if people without symptoms can pass it on , could this mean that any time you leave your house you might be exposed to the virus wafting through the air?
Health officials think yes. For example, in an update last week, Harvey Fineberg, MD, PhD, chairman of a committee with the National Academy of Sciences, said that COVID-19 (the illness associated with the new coronavirus) can spread via talking or even breathing.
"Some of us by talking or even breathing produce a number of these tiny bioaerosol particles, and those effectively can float around for a while," he explained further in an interview with NPR . He also pointed out that this is a problem mainly in enclosed spaces, like patient-care rooms. When you are outdoors and practicing social distancing, however, those particles get dispersed in the outside environment (like if they're blown around by the wind, for instance). "There's no real danger from that," he noted.
Because this is a brand-new coronavirus, the Centers for Disease Control and Prevention (CDC) acknowledges that "we are still learning how it spreads , the severity of illness it causes, and to what extent it may spread in the United States." So, yes, more research is needed for a definitive answer to this question, although infectious disease experts can shed some light on what they know so far about whether or not the novel coronavirus can spread through the air.
So...is the novel coronavirus airborne?
The short answer is: likely yes, but it's complicated. First, it's important to note that airborne can mean different things to different people, even experts. In general, a pathogen is considered airborne when it can spread via smaller particles that can remain in the air for long periods of time , says Natasha Bhuyan , MD, a specialist in infectious diseases and family physician in Phoenix, Arizona. The exact length of time that viral particles in general hang in the air before they dissipate depends on a variety of factors, including the temperature and humidity of the area, and so on, adds Rishi Desai , MD, a former epidemic intelligence service officer in the division of viral diseases at the CDC.
Now let's talk about the new coronavirus specifically: When someone who has novel coronavirus coughs or sneezes, the tiny droplets that come out of their nose and mouth are like a tiny cloud of mist—and it’s possible that they linger, says Dr. Desai. Experts just don't know the concrete answer at this point for how long, be it a few seconds or more like hours .
It's also not totally clear how far those particles travel, although current research suggests the virus can spread most easily when people are within about 6 feet of each other. You may have seen recent headlines that COVID-19 particles can reach as far as 23 to 27 feet away from the origin point, after researchers shared this info in an article published by JAMA . However, some health officials warn this is misleading , and that the current CDC guideline to stay 6 feet away from others still stands (more on that later).

Are there any guesses on how long new coronavirus particles can stay airborne?
In a study published March 18 in the New England Journal of Medicine , researchers found that SARS-CoV-2 (the virus that causes the COVID-19 illness) remained contagious in aerosols, like droplets from coughing, for three hours .
It's worth pointing out, though, that the experiments performed in this study (which also looked at SARS-CoV-2 viability on plastic, copper, and more, in addition to aerosols) were done in a highly controlled laboratory setting. But the authors concluded: "Our results indicate that aerosol ... transmission of SARS-CoV-2 is plausible, since the virus can remain viable and infectious in aerosols for hours."
So does the stay-6-feet-away rule still hold true?
Right now, yes. Particles may travel through and linger in the air simply by talking or breathing near someone, as Dr. Fineberg said in a government letter at the beginning of April. So, viral particles could hang around even without the force of a cough or sneeze behind them. This is why it's still so important to maintain a 6-foot distance from others, even when you're just casually chit-chatting with someone.
But even if a mist of the novel coronavirus hangs around for hours around where a person breathed, coughed, sang, spoke, etc., the CDC maintains that "airborne transmission from person-to-person over long distances is unlikely."
Dr. Bhuyan reiterates that message, saying you’re still most likely to catch it directly from an infected person when they expel droplets containing viral particles, and those particles land on your face, body, or a nearby surface (where you could potentially pick them up and then touch your face, for example)—or you're close enough to breathe them in. And again, we’re talking pretty tight person-to-person contact.
New research continues to emerge about how COVID-19 spreads—and there’s still a lot to learn . So, it's important to take all info with a grain of salt as new discoveries pop up.
If COVID-19 is airborne, should I wear a mask when I'm out and about?
As cases of novel coronavirus go up, health officials are starting to recommend the general public wears fabric masks when going out for essential activities, like grocery shopping, as WH reported previously .
Dr. Fineberg also explained in his NPR interview: "My answer right now is that it would be prudent for all of us when we're out and about to wear a face covering." But the main reason isn't to protect yourself; it's to protect others, he explained. Because you can spread the virus unwittingly if you're asymptomatic or pre-symptomatic, you want to reduce the risk of spreading it to others by staying physically distant and blocking potentially dangerous particles from escaping you (like with a homemade nose-and-mouth blocker ), even when you feel fine.
And I should still keep up with my other stay-safe measures, right?
You bet! Experts agree: The key to fighting this pandemic is reducing your exposure to the virus as much as you can. So keep doing what you’re probably already doing. Stay away from potentially sick people who may sneeze or cough (and if that’s you, stay at home to avoid spreading it and cover your mouth with your elbow or sleeve), make sure to clean and disinfect surfaces at home , wash your hands frequently (for at least 20 seconds!), and try to avoid touching your eyes, face, or mouth, says Dr. Desai.
When it comes to social distancing, remember the 6-feet rule (have you heard this enough times yet?); that’s the distance you need to keep between you and other people in order to reduce your risk of being exposed to the virus if they’re carrying it (even if they don't know it!). If you can avoid being in public places (e.g., the grocery store), do so. And if you do need to run errands, try to do them solo to avoid populating a shared space with more people than necessary.
As you settle in for the long haul, remember that everyone is in this together. And as backwards as it might seem, keeping a physical distance between you and others is one of the best ways you can show friends and family that you care, as well as the most at-risk for the novel coronavirus among us, including older people and those living with chronic conditions or compromised immune systems.

Novel Coronavirus

Here's What That Faint line On A COVID Test Means

Which COVID Vaccine Should I Get?

How Long Do COVID-19 Symptoms Last?
How Long Will I Test Positive For COVID?

New COVID Variant Boosters Explained By Experts

When Are You Most Contagious With COVID?

Will There Be A 'Tripledemic' In Fall 2023?

Will Covid Mask Mandates Return In 2023?

Best Disposable Face Masks To Buy On Amazon 2023
What To Know About BA.2.86 And EG.5 COVID Variants

‘COVID Triggered My Nervous System Disorder’
Appointments at Mayo Clinic
Ebola transmission: can ebola spread through the air, can ebola spread through the air.
No, the virus that causes Ebola is not transmitted through the air. Unlike a cold or the flu, the Ebola virus is not spread by tiny droplets that remain in the air after an infected person coughs or sneezes.
Ebola is spread between humans when an uninfected person has direct contact with body fluids of a person who is sick with the disease or has died. People become contagious when they develop symptoms.
Body fluids that can transmit Ebola include:
- Breast milk
- Vaginal fluids
- Pregnancy-related fluids
What is the path of transmission?
Research suggests that fruit bats are most likely the original hosts of the Ebola virus. Other animals that have been infected include chimpanzees, gorillas, monkeys, forest antelope and porcupines. There is no evidence that mosquitoes or other insects transmit the Ebola virus.
For humans, the source of exposure to virus-carrying body fluids may include:
- An infected animal
- Another person who has symptoms of the disease or has died from the disease
- Contaminated objects, such as clothing, bed linens, doorknobs, needles and other medical equipment, or other surfaces
After people have recovered, the virus can often be detected for many months in certain body fluids, including semen, breast milk and urine.
The virus enters a person through a break in the skin or through the mucous membranes, such as the tissues of the eyes, nose, throat or vagina. For example, you could become infected if you touched infected body fluids and then touched your eyes.
The time from infection to the appearance of symptoms (incubation period) is usually eight to 10 days but can range from two to 21 days.
Pritish K. Tosh, M.D.
- Infection: Bacterial or viral?
- Bray M, et al. Epidemiology and pathogenesis of Ebola virus disease. https://www.uptodate.com/contents/search. Accessed March 17, 2021.
- Ebola (Ebola virus disease): Transmission. Centers for Disease Control and Prevention. https://www.cdc.gov/vhf/ebola/transmission/index.html. Accessed March 17, 2021.
- AskMayoExpert. Viral hemorrhagic fever. Mayo Clinic; 2019.
- Ebola virus disease. World Health Organization. https://www.who.int/en/news-room/fact-sheets/detail/ebola-virus-disease. Accessed March 17, 2021.
- Bennett JE, et al. Marburg and Ebola virus hemorrhagic fevers. In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed March 17, 2021.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book
- Antibiotics: Are you misusing them?
- Childhood vaccines
- COVID-19: How can I protect myself?
- Enterovirus D68 and parechovirus: How can I protect my child?
- Hand-washing tips
- Infectious diseases
- Mayo Clinic Minute: What is the Asian longhorned tick?
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Mayo Clinic Minute: Will there be a Lyme disease vaccine for humans?
- Monkeypox: What is it and how can it be prevented?
- Vaccine guidance from Mayo Clinic
- Vaccines for adults
- What are superbugs and how can I protect myself from infection?
- What is chikungunya fever, and should I be worried?
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Ebola transmission Can Ebola spread through the air
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
" Effective MRSA Staph Treatment Options and Support Since 2008 "

- Information
- Recurring Infections
Airborne MRSA facts, risks and prevention
MRSA bacteria travel through the air on skin or dust particles from people who are infected, or from carriers.
It’s commonly known that MRSA is transmitted by touch, but few people are aware of another way this infection can spread: as airborne MRSA.
The risk of transmission of MRSA or Staph in the air is well established in many studies. However, neither the CDC MRSA hospital precautions nor the media is letting the public know about this problem. More importantly, hospitals and health care facilities aren’t publicizing this risk. I even know of doctors and RNs who have expressly denied that these infections can spread through the air.
Let’s look at how these bacteria become suspended in the air, what the risks are, and what the studies say about MRSA in the air. Then let’s review some techniques to help guard against germs floating in the air.
How and why does MRSA spread into the air?
First of all, there are two types of people who can spread this disease: 1) people who are infected and 2) people who are “ carriers ” but are not infected themselves.
Both types of people can be a source of airborne bacteria. This is because the average person sheds millions of skin particles throughout the day. Because these bacteria love the skin, they can hitch a ride on tiny skin particles that circulate into the air. Particles landing on other people can lead to colonization of their skin with the bacteria. If the particles are small enough, they can also enter the nose (also causing colonization) or lungs (possibly causing pneumonia).
Risks in hospital room air
Studies have been performed in hospitals to see how these infections move through the air. Their findings can help you understand the risks, whether you are in a hospital or at home.
- Studies have now confirmed that the in-air route of transmission is responsible for a large number of resistant Staph infections.
- A June 2001 study published in the JAMA Otolaryngology Head and Neck Journal, showed that MRSA could be acquired by medical staff and patients through the air in hospitals. The study was conducted in a hospital ward and found MRSA re-circulating in the air, among the patients and on inanimate objects in the area, especially when there was movement in the patient’s rooms. This study identified both colonized carriers and infected people as sources of risk. This study concluded that Methicillin-resistant S aureus was recirculated among the patients, the air, and the inanimate environments, especially when there was movement in the rooms. Measures should be taken to prevent the spread of MRSA in the air in order to control hospital acquired infections.
- A new study from Leeds University in 2012 shows that patients with MRSA can spread the bacteria into the air inside their rooms.The study used a heated mannequin inside a controlled chamber to simulate an infected patient in a hospital room. The bacteria were released from the mannequin and were detected up to 11 feet away inside the chamber.
You’re at increased risk when sharing or visiting hospital rooms

The Leeds University study highlighted the potential risk of catching MRSA in two-bed hospital rooms. If one of the patients in a room is infected, the other patient could come into contact the bacteria through the air. The 2001 study above also highlighted that people who were colonized (and not infected) also spread the bacteria into the air. The same risks apply to visitors or hospital workers who enter the room.
What’s more, the risk comes from the air itself, without direct contact with the infected patient or contaminated surfaces or objects. While MRSA air contamination is a risk in hospitals, the highest risk is still from direct person to person contact, or from touching contaminated surfaces or objects. So good hand washing and personal hygiene are still your best line of defense when visiting a hospital. But to protect yourself as well as possible, you should also be aware of the risk of bacteria in the air and take steps to reduce the risk, as outlined below.
Because standard cleaning and disinfection methods (both at home and in hospitals) only focus on contact surfaces, different precautions are needed to address airborne Staph and MRSA.
Prevention strategies for hospitals and caring for others
In hospitals: One of the best preventative measures for air bacteria is for hospitals to isolate infected patients (and for those who are simply colonized) to reduce the risk of the infection spreading. While some hospitals do this, many do not. Find out about the hospital’s policy on sharing rooms with MRSA patients and take extra precautions if you have to share a room with such a patient.
Stay clear of uncovered wounds, such as when dressings are being replaced. Do not touch anyone’s wounds or dressings. Wash your hands after visiting a hospital room.
When staying in a hospital, use a method to reduce bacteria in the air. This will reduce your chances for getting infected during your stay (see suggestions below).
Caring for others: Wash your hands after caring for wounds and infections. In-air bacteria can be present when caring for anyone who’s infected or who is colonized. Use techniques to reduce air bacteria if someone in your home is infected (see below).
How to reduce airborne bacteria
HEPA Filtration: A 2006 study in the UK looked at filtering the air in a hospital ward to see if they could reduce MRSA levels. They initially found that 95% of areas tested had measurable contamination. They used a portable HEPA filtration unit and found contamination decreased by 75%-90% in these same areas. The study researchers concluded that filtering the air is likely to reduce cross-infection risks significantly with little cost and effort.
There are many types of HEPA filtration units, and they have different airflow rates. However, it seems that running a portable HEPA filter either at home or in a hospital room could reduce the risks.
Many essential oils are antibacterial and thus you’ll see data showing many types of oils are active against bacteria. According to studies at Weber State University and at Wythenshawe Hospital, a simple and easy way to reduce the risk from bacteria in the air is to diffuse essential oils. This method has been shown to reduce many types of bacteria, including MRSA.
Wythenshawe Hospital Burns Unit in England found that using a vaporizer to diffuse a blend of oils into the air combated MRSA bacteria. They ran a 9 month study and found that in-air bacteria diminished by 90% and the number of hospital infections were also reduced.
Another study looked at the antibacterial activity of geranium and lemongrass oils over a range of concentrations by direct contact and by vapour diffusion using a hospital-grade diffuser. The study examined MRSA, VRE, and other superbugs. In an office environment, the diffuser provided an 89% reduction of these superbugs after 15 hours of use.
Many infectious diseases can spread in the air, including MRSA and Staph. While good hygiene and hand washing are crucial to protect against surface and direct contact risks, it also makes sense to reduce the risk of airborne germs settling on your skin or getting into your nose or lungs.
One of the easiest and most effective ways to control germs in home or hospital air is diffusing antibacterial essential oils. HEPA filtration can also be a help. Keeping isolated from people with active infections can also reduce the risk, where practical.

- See Tips on how to diffuse essential oils for reducing bacteria in the air
- Many people Carry Staph bacteria in their nose
- What are essential oils and how are they used for infections?
References:
1) Significance of Airborne Transmission of Methicillin-Resistant Staphylococcus aureus in an Otolaryngology–Head and Neck Surgery Unit; Teruo Shiomori, MD, PhD; Hiroshi Miyamoto, MD, PhD; Kazumi Makishima, MD, PhD; Arch Otolaryngol Head Neck Surg. 2001;127(6):644-648. https://archotol.jamanetwork.com/article.aspx?articleid=482358
2) Reduction in MRSA environmental contamination with a portable HEPA-filtration unit by TC Boswell & PC Fox Journal of Hospital Infection 2006 May;63(1):47-54. https://www.ncbi.nlm.nih.gov/pubmed/16517004
3) Fears over risk of air transmission of superbugs, BBC News Health Oct 12 2012, https://www.bbc.co.uk/news/health-19898735
4) Wythenshawe Hospital Burns Unit in England found that using a vaporizer to diffuse essential oils into the air combated the superbug MRSA. Essential oils ‘combat superbug’, 2007, BBC News, https://news.bbc.co.uk/2/hi/uk_news/england/manchester/6471475.stm
5) Vapour–phase activities of essential oils against antibiotic sensitive and resistant bacteria including MRSA, A.L. Doran, W.E. Morden, K. Dunn, V. Edwards-Jones. https://onlinelibrary.wiley.com/doi/10.1111/j.1472-765X.2009.02552.x/full

- Pictures of Staph and MRSA
- MRSA and Staph Symptoms
- How Contagious is MRSA?
- What is a MRSA Carrier?
- Natural Remedies Overview
- Essential Oils for Infections
- Our Products
- MRSA Secrets Revealed Program
- Customer Reviews
- How to Win the MRSA Battle
- Overcoming Staph
- 7 MRSA Facts and Myths
- Caring for a Loved One
- 3 Steps to Stop MRSA
- What Your Doctor Isn’t Telling You
- Testimonial Disclaimer
- Opt-Out Preferences
Medical Disclaimer: Michelle Moore is not a doctor or healthcare practitioner, but she is someone who overcame many health obstacles that traditional medicine could not solve. This information is based upon Michelle Moore’s scientific research, education and personal experience and it is for educational purposes only. Information in this web site has not been evaluated by the US Food and Drug Administration (FDA).
This information is not intended as medical advice, diagnosis or treatment. Always seek the advice of your physician with any questions you may have regarding any medical condition. When choosing a healthcare provider do your own research to ensure they are right for you.

We use cookies to enhance your browsing experience, serve personalized ads or content, and analyze our traffic. By clicking “Accept”, you consent to our use of cookies. Not consenting may adversely affect certain features and functions.
Can COVID-19 be transmitted through the air?
Medically reviewed by Drugs.com . Last updated on March 28, 2024.
Official answer
Yes, the new coronavirus SARS-CoV-2 can be transmitted through the air, but whether or not it is airborne is still a matter that experts are debating.
Transmitted through the air vs airborne - what’s the difference?
SARS-Cov-2 is thought to be primarily spread between people via infected respiratory droplets that are released when an infected person coughs, sneezes or exhales. These droplets are most likely to infect people in close proximity (within 6 feet) via a process called droplet transmission.
Given that the infected respiratory droplets are moving through the air before infecting someone else, many people might be wondering why we’ve been told the virus isn’t airborne. Scientists, however, consider airborne transmission to be different from droplet transmission and this all comes down to the size of the droplets being spread.
Droplets greater than 5-10 m in diameter are considered to be respiratory droplets and even though they can spread through the air they are not considered to be ‘airborne’. Droplets (or aerosols) smaller than 5 um in diameter, called droplet nuclei, can remain in the air for longer periods of time and travel further distances. This type of droplet is said to be airborne.
Is it possible that SARS-CoV-2 is actually airborne?
On March 27, 2020, the World Health Organization (WHO) indicated that in certain circumstances airborne transmission of SARS-CoV-2, the new coronavirus that causes COVID-19, is possible. This might occur when, for example, a patient is being intubated or using a nebulizer because aerosols containing the virus could be generated during these procedures.
Scientists have also been investigating the possibility that SARS-CoV-2 could be airborne, but the research is still limited and some research does not show that the virus is airborne. The evidence, however, seems to be growing in favor of the possibility that it may be.
On April 1, 2020, the US National Academy of Sciences (NAS) sent the White House a letter, which acknowledged that limited research had been conducted, but which also stated that “the results of available studies are consistent with aerosolization of virus from normal breathing”.
The letter from the NAS highlights the results of a study conducted at the University of Nebraska Medical Center, which suggested that viral aerosol particles are produced by patients with COVID-19, even when they do not cough. Further experiments are ongoing to determine the viral activity of the viral aerosol particles produced by such patients. Low concentrations of virus were recovered from the samples obtained during the study, making it difficult to determine if virus in the particles was capable or likely to cause infection in another person.
Help stop the spread of COVID-19
Preliminary evidence suggests SARS-CoV-2, may be airborne, although further research is necessary to fully understand how the virus spreads. In the meantime, to help stop the spread of COVID-19, make sure that when you’re indoors the areas you are in are well ventilated. Opening windows or doors can help improve ventilation. And, if you’re out in public then follow the US Centers for Disease Control and Prevention’s (CDC) advice and wear a facemask.
Related questions
- Can you have Covid without a fever?
- Which breathing techniques help with COVID-19?
- Is Omicron worse than Delta?
- World Health Organization (WHO). Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. March 27, 2020. [Accessed April 7, 2020]. Available online at: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations .
- The National Academy of Sciences. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic. April 1, 2020. [Accessed April 7, 2020]. Available online at: https://www.nap.edu/read/25769/chapter/1 .
- Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. Published online March 4, 2020. doi:10.1001/jama.2020.3227.
- Santarpia JL, Rivera DN, Herrera V, et al. Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center. medRxiv [Accessed April 7, 2020]. doi: https://doi.org/10.1101/2020.03.23.20039446 .
- Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 (COVID-19). How to Protect Yourself & Others. [Accessed April 7, 2020]. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html .
Can you become immune to COVID-19?
Patients who recover from COVID-19 make antibodies to the virus that may impart immunity for at least 6 months; however, breakthrough infections do occur and may be more likely with newly circulating variants of the virus. Immunizing with the latest recommended COVID-19 vaccine can help to extend your immunity and prevent disease. Continue reading
Is obesity a major risk factor for Covid-19?
Obesity is a major risk factor for covid-19 and people who are obese are more likely than those who are not obese to contract Covid-19 at a younger age, develop severe Covid-19, require hospitalization, oxygen, mechanical ventilation, intubation, or admission into ICU, end up in hospital sooner, or die from Covid-19. Continue reading
COVID-19 vaccines and variants: What you should know
The top 3 SARS-CoV-2 variants in the U.S. in early December 2023 are all of Omicron lineage and include: HV.1 (30%), JN.1 (21%) and EG.5 (9%). Currently the JN.1 variant is increasing, while HV.1 seems to be decreasing. These percentages are based on modeled predictions of variant proportions. Continue reading
Related medical questions
- How effective is Lagevrio (molnupiravir) for COVID-19?
- COVID-19: Why is social distancing so important?
- Should I wear a face mask to protect myself from COVID-19?
- Why do more men die from coronavirus?
- Can Ivermectin be used to treat COVID-19?
- Can you take Ibuprofen if you have COVID-19 (coronavirus)?
- What antibiotics kill Covid-19 (coronavirus)?
- COVID-19: What are the Stages and Causes of Death?
- What's the difference between Bacteria and Viruses?
- Does Zinc protect you from Covid-19 or boost your immune system?
- Does Losartan block the receptor used by the Coronavirus?
- An Update: Is hydroxychloroquine effective for COVID-19?
- How do I Treat Nasal Congestion with COVID-19?
- Where can I buy an at-home test kit for COVID-19 (coronavirus)?
- Can you take Paxlovid twice if COVID rebounds?
- Does Mucinex help with Covid?
- Does Tamiflu (oseltamivir) work on COVID-19?
- Can vitamin C prevent or treat COVID-19 (coronavirus)?
- Should I take Paxlovid after a Positive COVID-19 Test?
- How long does COVID-19 last? and other COVID-19 FAQ
- Can I take NyQuil with COVID or after the COVID vaccine?
- How effective is Paxlovid for COVID-19?
- Do ACE inhibitors make COVID-19 worse?
- Can you take Ibuprofen after the COVID booster vaccine?
- Does Paxlovid prevent Long COVID?
- Does methylprednisolone help with COVID?
- Can NSAIDs be used to treat a COVID-19 fever?
- What are JAK inhibitors and how do they work?
- Can Colchicine be used to treat COVID-19 (coronavirus)?
- Does the BCG vaccine for TB help with COVID-19 (coronavirus)?
Related support groups
- COVID-19 (103 questions, 87 members)
Medical Disclaimer
Watch CBS News
Indoor air systems crucial to curbing spread of viruses, aerosol researchers say
By Jon LaPook
Updated on: June 30, 2024 / 7:00 PM EDT / CBS News
This is an updated version of a story first published on Oct. 29, 2023. The original video can be viewed here .
With new strains of COVID continuing to appear, and flu season just months away, we thought now is a good time to consider what the pandemic has taught us about preventing the spread of potentially deadly respiratory infections.
It turns out, viruses like the one that causes COVID-19 can travel much farther than six feet. So public health advice focusing on social distancing, handwashing, and masking wasn't enough. Air quality scientists say, from the start of the pandemic , it also should have focused on improving the air we all breathe … indoors.
As we first reported last fall, some companies are now doing just that – for the health of their workers and the health of their bottom line.
Joe Allen: The original sin of the pandemic was the failure to recognize airborne transmission.
Professor Joe Allen of Harvard's T.H. Chan School of Public Health believes the rapid spread of COVID in early 2020 was preventable.
Joe Allen: Think about the public health gains we've made over the past hundred years. We've made improvements to water quality, outdoor air pollution, our food safety, we've made improvements to sanitation: absolute basics of public health. Where has indoor air been in that conversation? It's totally forgotten about. And the pandemic showed what a glaring mistake that was.

Dr. Jon LaPook: What do you think was lost because of that lag in understanding of how this was spread?
Joe Allen: Tens of thousands of lives in the U.S., many more globally. It's not an exaggeration.
It's also no exaggeration to say those early days of COVID were unforgettable. In the U.S. by March 2020, the virus began taking its toll in places like the Life Care Center nursing home in Kirkland, Washington. Sixty miles away in Mount Vernon, Washington, the Skagit Valley Chorale held one of its weekly rehearsals in a church. Half the members stayed away. But the other half showed up. Among them were board members Debbie Amos, Mark and Ruth Backlund, and Coizie Bettinger.
Coizie Bettinger: We just thought hand sanitizer, wash your hands a lot, you know, don't hug each other, 'cause that's touch.
None of it was good enough. Within a few days, chorale members began to get sick. In all, COVID hit 53 of the 61 people there that night. Two of them, both in their 80s, died.
Ruth Backlund: We were going, "This-- this has got to be spread some other way." It--
Dr. Jon LaPook: Really?
Ruth Backlund: Because we were good. We were good.
Dr. Jon LaPook: So COVID was percolating and you thought you were doing everything you were supposed to do?
Marck Backlund: Yes.
Debbie Amos: Right.

Skagit County health officials said the rehearsal "could be considered a superspreading event" – one of the earliest in the country – and concluded that choir members had "an intense and prolonged exposure" to surfaces, droplets and possibly even microscopic airborne particles called "aerosols," containing the virus. That caught the attention of Linsey Marr, a Virginia Tech university professor specializing in aerosol science, and several of her fellow researchers. Even though the medical community was focused on droplets, surfaces and handwashing, these researchers strongly believed COVID was mostly an airborne disease, but needed more proof. So they launched their own analysis.
Linsey Marr: I thought, "Wow. This is even worse than I thought "This has to be airborne. There's really no other explanation for it." Some people are gonna say, "Oh, they all touched the same doorknob." But, after the first few people touch that doorknob, there's no more virus left.
Linsey Marr: That's what happens with our exhaled breath.
Professor Marr used a portable fogger to help explain how so many choir members could have gotten sick.
Linsey Marr: When they're singing, they are releasing virus particles into the air constantly, probably, like this. And those are going to drift around in the room. Notice they're not just falling to the ground. And now as we continue to sing, there's more and more of them in the room. And you can see, as they're drifting around they're reaching these other people nearby. And they were there for two and a half hours. And you can imagine that after that amount of time the other people would've breathed in enough of them to get sick themselves.
Dr. Jon LaPook: Especially if at night the HVAC system was turned off.
Linsey Marr: As far as we know, it wasn't running and so there were very – there was very poor ventilation in that room when this was all happening.
An HVAC unit, short for heating, ventilation and air conditioning, is the heart and lungs of any building. The researchers suspected the thermostat most likely shut off the HVAC unit because the chorale members were generating enough heat on their own.
Dr. Jon LaPook: And right now, there's no ventilation?
Linsey Marr: Very, very low.
Dr. Jon LaPook: OK.
Linsey Marr: And actually, it's similar to what was in the church where the group was rehearsing.
Then, Professor Marr turned up the circulation to show us how better air flow could have helped remove aerosols and slow the spread of virus.

Linsey Marr: Instead of just drifting all over the room --
Dr. Jon LaPook: Oh…
Linsey Marr: You can actually see it, right, going up through there--
Dr. Jon LaPook: I sure can. That is dramatic to see that.
The analysis led to one of the most significant papers on the importance of ventilation published during the pandemic. Then, in 2022, a study in Italy went further. It found that by using a school's fans and air ducts to mechanically exchange indoor air with outdoor air five times an hour, the risk of COVID-19 infections decreased by at least 80 percent. But, in the U.S. it took until May of 2023 for the CDC to recommend an air exchange rate at all.
Joe Allen: If you look at the way we design and operate buildings, and I mean offices, schools, local coffee shop, we haven't designed for health. We have bare minimum standards. In schools the minimum air change, by design, is about three air changes per hour. Remember, we want at least four to six.
Dr. Jon LaPook: If we'd had these indoor air quality targets before the pandemic, how do you think the pandemic would have unfolded differently?
Joe Allen: We still would have had spread. This isn't an "end-the-pandemic" thing. We would have had a lot less of it, and we would have a lot less of these superspreading events. Think about the early days of the pandemic, with "flatten the curve"---"stay home." Why wasn't "Improve indoor air quality" part of "flatten the curve"? We had tools to protect ourselves. Masking: great tool, it's a filter. But we ignored the building side of this.
- Face mask effectiveness: What science knows now
Buildings are Allen's business. As the founder of Harvard's Healthy Buildings program, he diagnoses problems in air quality systems and comes up with solutions for clients that include CBS's parent company, Paramount, and commercial real-estate companies like Beacon Capital Partners, with buildings like this one in downtown Boston. And, he advised Amazon before these new 22-story towers opened last year in Arlington, Virginia, where he gave us a tour.
Dr. Jon LaPook: What does a state-of-the-art building look like in terms of air?
Joe Allen: We see a lot of the elements in this building. You have a dedicated outdoor air system that's delivering air above the minimum requirements. Then it's going through two MERV-13 filter banks, and you have highly filtered air.
MERV stands for minimum efficiency reporting value. A rating of 13 means it catches up to 90 percent of airborne particles… depending on their size… as the first line of defense not just against COVID, but other airborne respiratory viruses like flu and RSV.

Joe Allen: This is the part of the building nobody ever sees. But this determines whether or not you're healthy or sick in the building, really, what happens in this space.
At Amazon's new offices, the top floor is a maze of motors, pipes, and air ducts… part of a $2.5 million HVAC system that begins with massive rooftop vents and dampers.
Joe Allen: Right here, this is the whole air handling system. This is where the air comes into the building, it's filtered, it's cooled, and then delivered. This determines how much air actually reaches the office space where people are working, and how clean that air is.
Downstairs, each floor has a sensor that tells building engineers about the quality of the indoor air … such as levels of carbon dioxide, known as CO2.
Dr. Jon LaPook: We breathe out the carbon dioxide.
Joe Allen: That's right
Dr. Jon LaPook: The less carbon dioxide, the better the ventilation?
Joe Allen: Really straightforward. High carbon dioxide means you're not getting enough outdoor air from that system we just looked at. If it's low, you're in good shape. Then we also measure particles. That tells us things about, like, outdoor air pollution.
The entire system can be monitored and controlled from the basement.
Joe Allen: Remember we talked about carbon dioxide is an indicator for ventilation? Well, I can see in this building all of these are under 800 parts per million.
Dr. Jon LaPook: So that's good?
Joe Allen: That's great. And really important: if a lot of people went into a space, the CO2 level would rise, this system would recognize it. The dampers would open up and bring in a lot more outdoor air.
Katie Hughes, Amazon's director of health and safety, pointed to the waves of wildfire smoke that have swept down from Canada as the ultimate test of the indoor air quality system.
Dr. Jon LaPook: Not too long ago, Washington and Virginia were sort of smothered by this smoke coming down from Canada. What happened in this building?
Katie Hughes: You would expect the air quality within the facility to not be great. Our buildings were performing very well.
Amazon says it has updated and continues to monitor its HVAC systems…including in its warehouses.
A recent survey of facility managers in the U.S. and Canada found that since March 2020, roughly two-thirds of respondents have upgraded their MERV filters and increased their air exchange rates. In New York City, JPMorgan Chase says its new headquarters will have state of the art air quality controls. And this new skyscraper called 1 Vanderbilt already runs a modern HVAC system.
Katie Hughes: COVID shifted everybody's mindset in terms of air quality in terms of communicable or infectious diseases.
Dr. Jon LaPook: Are you finding that Amazon is making a business decision partially by saying, "Look, it's okay for you to come back to work, because we're telling you that the air inside this building is safe"?
Katie Hughes: I think it's one of many reasons why we expect or would like people back in the office. That is-- a good thing to have, it's probably one of many things.
A well-operating HVAC system is not only good for the health of employees. It can be good for the health of companies, too, especially with people working remotely, leaving many commercial building owners looking for tenants.
Dr. Jon LaPook: There's empty office space, in New York City and elsewhere. How do you think this new thinking might affect that in terms of people even wanting to come to work?
Joe Allen: The dynamic has changed: It's a total buyers' or tenants' market. All else equal, which building are you gonna go to? You have your choice right now: This building that put in healthy building controls, or this building that's designed the way we've always designed buildings, and is prone to being a sick building?
Dr. Jon LaPook: So it actually can help the bottom line in addition to, of course, improving health?
Joe Allen: Yeah.
Dr. Jon LaPook: What about retrofitting a building that's old?
Joe Allen: I think it's a misconception that old buildings can't be healthy buildings. Some of these fixes don't take much. Improving the level of filtration? That's easy; it's cheap; protects against COVID-19; influenza; also protects against wildfire smoke and outdoor air pollution; protects against allergens. Simple, absolute basic things that can be done.

The Skagit Valley Chorale rehearsals are now in a different church with a new HVAC system. For the last year, doors were left open to let in fresh air, regardless of the season, and there are even portable carbon dioxide monitors to track ventilation.
Debbie Amos: We've been through a traumatic experience. And we've tried to learn from that. And did help the science with the aerosol study. And now, we're moving on in a way that we can still sing-- but in a more safe manner.
Dr. Jon LaPook: Do you worry that when the spotlight of the pandemic starts to fade, that people will forget and that they won't act the way they should, in terms of buildings?
Joe Allen: I'm a bit more optimistic than that. I think there are fundamental shifts that have happened. The scientific and medical literature's being rewritten. The government and standard setting bodies are setting new health-based standards. Businesses are responding and won't forget what this meant to their employees' health, and their business. So I don't think we're gonna forget these lessons. We better not.
Produced by Andrew Wolff. Associate producer, Tadd J. Lascari. Broadcast associate, Eliza Costas. Edited by Matt Richman.

Jon LaPook, M.D. is the award-winning chief medical correspondent for CBS News, where his reporting is featured on all CBS News platforms and programs. Since joining CBS News in 2006, LaPook has delivered more than 1,200 reports on a wide variety of breaking news and trending stories in the health and medical fields, as well as feature stories on music, lifestyle and profiles of entertainment stars.
More from CBS News

United Airlines texts customers live radar maps during weather delays

9 best long-term CDs for July 2024 (up to 4.80% APY)

5 ways seniors can boost their income this July

6 crucial questions to ask before consolidating your credit card debt
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Is the Flu Airborne?
Some flu spreads through close contact, but there's some other transmission too.
- Flu Transmission Explained
- When You’re Contagious
- Staying Ahead of the Flu
Frequently Asked Questions
Influenza , more commonly known as the flu, is most often spread when a person comes into contact with droplets or aerosols that contain mucus from an infected person.
Some research shows that approximately half of flu cases may stem from airborne transmission. Knowing how the flu is spread and understanding flu transmission can help you prevent infection and minimize your risk.
This article will discuss how flu is spread, including how long the flu is contagious and the flu incubation period. It will explain the difference between droplets and airborne spread, and how that might affect transmission.
Hiraman / Getty Images
Flu Transmission Explained
The flu is a virus that is most often spread when someone comes into contact with droplets from an infected person. These droplets are produced when a person with the flu coughs or sneezes, spreading infected mucus around them for up to 6 feet.
Droplets vs. Aerosols
Droplets are heavy. They generally sink to the ground within about 6 feet of the infected person. That means if you stay more than 6 feet away, you are less likely to become infected. Scientists believe that most flu transmission happens when a person inhales these droplets or enters their eye, nose, or mouth.
Aerosols are produced by coughing or sneezing, just like droplets. However, they are smaller and lighter, so they float in the air longer.
If the flu is airborne, that means the infectious virus can spread even if you stay more than six feet away. Researchers are still unclear about how much of the flu is spread via airborne transmission, but one study indicates that at least half of transmission happens via airborne particles.
Through Human Contact
When you’re close to someone, you’re more likely to come into contact with their respiratory secretions, such as mucus from the upper respiratory tract. The flu virus can also live on the skin of someone who has the virus, when these respiratory droplets or other bodily fluids fall to the skin. When you come into contact with these fluids, you can be exposed to the flu virus and contract influenza.
On Surfaces
Occasionally, the flu can be spread when you touch a surface that has the virus on it, then touch your own eyes, nose or mouth, allowing the virus to enter your body. This is called surface transmission. The flu can survive for up to 48 hours on hard objects like doorknobs. It survives for a shorter time on cloth and other porous surfaces.
When You’re Contagious
After you’ve come into contact with the virus, you can develop symptoms anywhere from one to four days later. You can begin spreading the flu one day before symptoms appear. You’re contagious for up to seven days, but most likely to infect someone else in the first three to four days of illness.
Staying Ahead of the Flu
The best way to prevent the flu is by getting vaccinated with a flu vaccine and practicing good hygiene, including washing your hands frequently. To reduce your chances of contracting the flu:
- Get vaccinated annually
- Wash your hands frequently
- Minimize contact with infected people, where possible
- Stay home when you are sick
- Avoid touching your nose, mouth or eyes, particularly in public
- Lead an overall healthy lifestyle
Flu Season and COVID Prevention
During the COVID-19 pandemic, there has been a dramatic decrease in flu cases, especially during the 2020-2021 flu season.
Researchers believe that this is largely due to COVID-related precautions including social distancing affecting flu rates. Flu activity rose during the 2021-2022 flu season, but preliminary estimates from the CDC show that there were fewer hospitalizations and deaths than in previous flu seasons. However, as some of the COVID-related precautions have been lowered since then, researchers predict upcoming flu seasons to be more severe.
Influenza is primarily spread through airborne transmission via aerosols. These tiny particles are released when an infected person coughs, sneezes or talks and can float through the air for a long time. However, research indicates that some transmission of the flu happens from coming into contact with an infected surface.
A Word From Verywell
Scientists are still studying how, precisely, the flu is spread. However, they know that certain precautions—including getting vaccinated and frequently washing your hands—can reduce the risk for flu transmission. Many of the same precautions that people have adopted to prevent the spread of COVID can also reduce your risk of spreading or contracting influenza.
The flu and COVID are both viruses that are passed by coming into contact with respiratory secretions from an infected person. However, COVID appears to spread more easily than the flu, including through aerosols. In addition, people with COVID can be contagious for a longer time before they start exhibiting symptoms, which may contribute to the spread.
The CDC maintains that most flu transmission happens from droplets, which stay within 6 feet of the infected person. However, research indicates that up to 50% of flu transmission may happen via aerosols.
Getting the seasonal flu vaccine reduces your risk of contracting the flu by 40%-60%, depending on the year. It also reduces your risk of hospitalization or death from the flu. All Americans who are 6 months or older unless advised otherwise by their healthcare provider can get the flu vaccine to reduce their risk of contracting the flu.
Centers for Disease Control and Prevention. How flu spreads .
Cowling BJ, Ip DKM, Fang VJ, et al. Aerosol transmission is an important mode of influenza A virus spread . Nat Commun . 2013;4:1935. doi:10.1038/ncomms2922
Centers for Disease Control and Prevention. How To Clean and Disinfect Schools To Help Slow the Spread of Flu .
Centers for Disease Control and Prevention. Healthy habits to prevent the flu .
Centers for Disease Control and Prevention. 2020-2021 Flu Season Summary .
Centers for Disease Control and Prevention. Past Seasons Estimated Influenza Disease Burden .
Ali ST, Lau YC, Shan S, et al. Prediction of upcoming global infection burden of influenza seasons after relaxation of public health and social measures during the COVID-19 pandemic: a modelling study . Lancet Glob Health . 2022;10(11):e1612-e1622. doi:10.1016/S2214-109X(22)00358-8
Centers for Disease Control and Prevention. Similarities and differences between flu and COVID-19 .
Centers for Disease Control and Prevention. Vaccine effectiveness: how well do flu vaccines work?
By Kelly Burch Burch is a New Hampshire-based freelance health writer with a bachelor's degree in communications from Boston University.
UK Edition Change
- UK Politics
- News Videos
- Paris 2024 Olympics
- Rugby Union
- Sport Videos
- John Rentoul
- Mary Dejevsky
- Andrew Grice
- Sean O’Grady
- Photography
- Theatre & Dance
- Culture Videos
- Fitness & Wellbeing
- Food & Drink
- Health & Families
- Royal Family
- Electric Vehicles
- Car Insurance Deals
- Lifestyle Videos
- UK Hotel Reviews
- News & Advice
- Simon Calder
- Australia & New Zealand
- South America
- C. America & Caribbean
- Middle East
- Politics Explained
- News Analysis
- Today’s Edition
- Home & Garden
- Broadband deals
- Fashion & Beauty
- Travel & Outdoors
- Sports & Fitness
- Sustainable Living
- Climate Videos
- Solar Panels
- Behind The Headlines
- On The Ground
- Decomplicated
- You Ask The Questions
- Binge Watch
- Travel Smart
- Watch on your TV
- Crosswords & Puzzles
- Most Commented
- Newsletters
- Ask Me Anything
- Virtual Events
- Betting Sites
- Online Casinos
- Wine Offers
Thank you for registering
Please refresh the page or navigate to another page on the site to be automatically logged in Please refresh your browser to be logged in
Flying Hippos: UK researchers find giant animal can become airborne
Trotting hippos can push limits of what we thought land animals could do, article bookmarked.
Find your bookmarks in your Independent Premium section, under my profile

Sign up for a full digest of all the best opinions of the week in our Voices Dispatches email
Sign up to our free weekly voices newsletter, thanks for signing up to the voices dispatches email.
Hippopotamuses are among the largest land animals and can often weigh more than 2,000 kilograms.
So it will come as a shock to many that they can become airborne.
They are most often pictured gliding through the water or lazing on a bank , but new research suggests the giant land creatures can become airborne for substantial periods of time.
When trotting fast, their feet leave the ground for up to 0.3 seconds at a time, a new study has found.
Research from the Royal Veterinary College (RVC) also suggests that unlike most large land animals, hippos almost exclusively trot, with the fastest ones taking to the air.
The findings suggest they are able to push the apparent limits of what giant land animals can do, even though they are amphibious.
Researchers say the findings will improve the understanding of how the size of large animals influences their movement on land.
Previous studies have suggested the animals often use a standard four-footed (quadrupedal) walk, with a footfall sequence of left hind, left fore, right hind, right fore – similar to elephants.
But other studies have claimed they trot with their diagonal feet in moving simultaneously.
Before now, researchers have not identified whether hippos become airborne when they move quickly, as is the case with other mammals, such as horses, but less common among larger animals.

John Hutchinson, Professor of evolutionary biomechanics and lead author of the study, said: “It’s hard to work with hippos as they tend to stick to the water and very seldom are trained to be studied in zoo collections.
“They’re also very dangerous. That’s part of the reason why science knew little about how hippos move before our research.
“We’re thrilled to provide the first study purely focused on revealing how hippos walk and run.
“We were pleasantly surprised to see how hippos get airborne when they move quickly – it’s really impressive.”
Prof Hutchinson and former RVC undergraduate student Emily Pringle collected video footage from Flamingo Land Resort in North Yorkshire, recording how two hippos moved in their paddock during the day.
They also sourced video footage from the internet of hippos moving, providing a broader range of behaviour and movements compared to those in captivity.
Analysing the data, they found that unusually for land animals, hippos almost exclusively trot – even when slowly walking or quickly running.
The study is published in the journal PeerJ.
Other land animals tend to have a wider range of gaits – for example, rhinoceroses can use a standard quadrupedal walk, trotting and galloping as they increase speed, much like a horse.
Elephants can only do typical walking (not trotting) and never leave the ground with all four feet, but can still run quickly.
The research will support the reconstruction of the evolutionary biomechanics of hippo lineages and help veterinarians diagnose or monitor hippos that have problems moving or are experiencing lameness.
Kieran Holliday, science and conservation officer at Flamingo Land Resort, said: “Understanding more about the species we work with will only help us to improve the care we can give them in the future, and the fact that this paper has uncovered possible new discoveries into hippo locomotion could have positive impacts to the wider zoo community in regards to husbandry and enclosure design.”
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
New to The Independent?
Or if you would prefer:
Want an ad-free experience?
Hi {{indy.fullName}}
- My Independent Premium
- Account details
- Help centre

IMAGES
VIDEO
COMMENTS
UC San Diego develops computer model to aid understanding of how viruses travel through the air. In May 2021, the Centers for Disease Control officially recognized that SARS-CoV-2 —the virus that causes COVID-19 —is airborne, meaning it is highly transmissible through the air.. Now University of California San Diego Professor and Endowed Chair of Chemistry and Biochemistry Rommie Amaro ...
Why the WHO took two years to say COVID is airborne. Early in the pandemic, the World Health Organization stated that SARS-CoV-2 was not transmitted through the air. That mistake and the prolonged ...
"The descriptor 'through the air' can be used in a general way to characterize an infectious disease where the main mode of transmission involves the pathogen travelling through or being ...
The World Health Organization is opening up the definition of airborne pathogens - such as Covid-19, influenza and measles - to include when respiratory droplets spread through the air and ...
Under this terminology, COVID-19 would be recognized as spreading through the air by airborne inhalation/transmission, with a much smaller risk of transmission by direct deposition. Up in the air
Airborne diseases can travel distances greater than 6 feet and remain infectious in the air from minutes to hours. This largely depends on the type of ventilation and preventative measures inside ...
The Centers for Disease Control and Prevention (CDC) is acknowledging COVID-19 can be spread through airborne transmission. The World Health Organization has recognized airborne transmission as a possibility since July. The CDC says larger respiratory droplets are more likely to spread COVID-19 than the small aerosols spread via airborne ...
But the potential for transmission depends on many factors, including infectiousness, dose and ventilation. New coronavirus is known to be spread via large droplets that fall to the ground. But ...
Experts can't agree. The World Health Organization says the evidence is not compelling, but scientists warn that gathering sufficient data could take years and cost lives. Some scientists say ...
An airborne virus was widely considered to be a germ that could travel in tiny particles called aerosols that hang suspended in the air and linger for quite a while, potentially traveling long ...
Droplets or aerosols. This is the most common transmission. When an infected person coughs, sneezes, or talks, droplets or tiny particles called aerosols carry the virus into the air from their ...
Airborne diseases pass from one person to another when microorganisms travel through the air. Chickenpox, the common cold, and COVID-19 are examples of airborne diseases.
But experts in how viruses can travel through the air say the CDC guidance doesn't emphasize enough that transmission at close range can also be through airborne particles, especially since ...
"There is growing evidence that droplets and airborne particles can remain suspended in the air and be breathed in by others, and travel distances beyond 6 feet (for example, during choir ...
It is intended to be posted outside rooms of patients with an infection that can spread through airborne transmission. ... Indoor respiratory secretion transfer data suggest that droplets/aerosols in the 20 μm size range initially travel with the air flow from cough jets and air conditioning like aerosols, ...
An "airborne" virus, in contrast, has long been considered to be a virus that spreads in exhaled particles that are tiny enough to linger in the air and move with air currents, letting them be ...
For a virus to be airborne means that it can be carried through the air in a viable form. For most pathogens, this is a yes-no scenario. ... does not travel long distances or remain viable ...
Recent research suggests that contagious novel coronavirus particles can linger in the air for a few hours. Health officials recently said that new coronavirus particles can become airborne from ...
No, the virus that causes Ebola is not transmitted through the air. Unlike a cold or the flu, the Ebola virus is not spread by tiny droplets that remain in the air after an infected person coughs or sneezes. Ebola is spread between humans when an uninfected person has direct contact with body fluids of a person who is sick with the disease or ...
Many infectious diseases can spread in the air, including MRSA and Staph. While good hygiene and hand washing are crucial to protect against surface and direct contact risks, it also makes sense to reduce the risk of airborne germs settling on your skin or getting into your nose or lungs. One of the easiest and most effective ways to control ...
Droplets greater than 5-10 m in diameter are considered to be respiratory droplets and even though they can spread through the air they are not considered to be 'airborne'. Droplets (or aerosols) smaller than 5 um in diameter, called droplet nuclei, can remain in the air for longer periods of time and travel further distances.
Indoor air systems "absolutely key" in curbing spread of viruses | 60 Minutes 13:20. This is an updated version of a story first published on Oct. 29, 2023.
Summary. Influenza is primarily spread through airborne transmission via aerosols. These tiny particles are released when an infected person coughs, sneezes or talks and can float through the air for a long time. However, research indicates that some transmission of the flu happens from coming into contact with an infected surface.
They are most often pictured gliding through the water or lazing on a bank, but new research suggests the giant land creatures can become airborne for substantial periods of time.
Human beings weren't designed to fly through the sky at 40,000 feet in a pressurized metal tube - with our aching limbs, burbling gastric systems and willful propensity to annoy other airborne ...